Understanding Splenic Vein Thrombosis: A Comprehensive Clinical and Radiologic Insight
Introduction
Splenic vein thrombosis (SVT) is an uncommon yet clinically important vascular disorder that is frequently overlooked in routine practice. Most cases are closely linked to underlying pancreatic diseases, particularly pancreatitis. Early and accurate recognition is essential, especially in patients who present with unexplained splenomegaly or signs of upper gastrointestinal bleeding. This in-depth article provides a comprehensive, expert-level review of SVT, covering its etiology, pathophysiology, epidemiological trends, clinical manifestations, diagnostic imaging features, treatment approaches, and long-term prognosis. It is designed as a valuable resource for radiologists, gastroenterologists, and other healthcare professionals involved in abdominal and vascular diagnostics.
What Is Splenic Vein Thrombosis?
Splenic vein thrombosis refers to the formation of a blood clot within the splenic vein, leading to venous outflow obstruction and potentially life-threatening complications such as gastric variceal bleeding.
Etiology: What Causes Splenic Vein Thrombosis?
SVT typically arises due to:
-
Pancreatitis (Acute or Chronic): The most common cause; inflammation from pancreatitis extends to the splenic vein, inducing endothelial damage and thrombosis.
-
Pancreatic neoplasms: Tumors may directly compress or invade the splenic vein.
-
Trauma or Surgical Interventions: Post-surgical or traumatic injury to the splenic vein may precipitate thrombus formation.
-
Portal hypertension and cirrhosis Can increase venous pressure and stagnate blood flow within the splenic vein.
Pathophysiology: How Does It Happen?
Obstruction of the splenic vein leads to retrograde congestion in collateral veins, most notably, the short gastric and left gastroepiploic veins. This causes:
-
Splenomegaly due to venous congestion.
-
Gastric varices, particularly in the fundus, may bleed.
-
Hypersplenism leading to thrombocytopenia and mild anemia.
Epidemiology
-
Incidence: Occurs in 5–22% of patients with pancreatitis.
-
Demographics: More common in males; typically affects individuals aged 40–60.
-
Association: Strongly associated with chronic pancreatitis, especially in alcohol-induced cases.
Clinical Presentation
Most patients are asymptomatic, and SVT is often an incidental finding. When symptomatic, the following may occur:
-
Upper gastrointestinal bleeding due to isolated gastric varices.
-
Left upper quadrant abdominal pain
-
Splenomegaly
-
Thrombocytopenia secondary to hypersplenism
Radiologic Features: How Is It Diagnosed?
CT Imaging (Preferred Modality)
Shows a filling defect in the splenic vein.
-
Often reveals associated pancreatic pathology such as inflammation or mass.
-
May demonstrate collateral veins and splenomegaly.
MRI
Useful for characterizing thrombus signal intensity and age.
-
MR angiography can assess the entire portal venous system.
Doppler Ultrasound
Non-invasive but operator-dependent.
-
May show absent flow in the splenic vein or turbulent flow in collateral vessels.
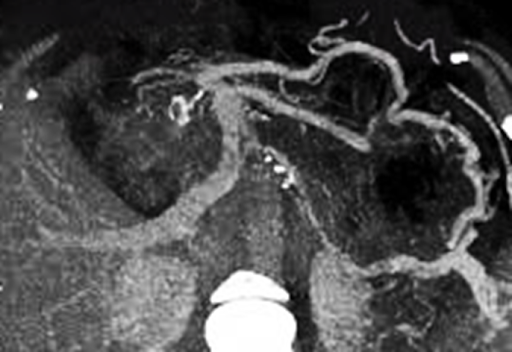
Featured Case Image:
The attached contrast-enhanced CT image demonstrates an occlusive thrombus in the splenic vein with surrounding pancreatic inflammation, consistent with pancreatitis-induced SVT.
Treatment Options
1. Observation
-
Asymptomatic patients without variceal bleeding can be monitored.
2. Anticoagulation Therapy
-
Used selectively in patients without active bleeding risk.
3. Splenectomy
-
Recommended for patients with recurrent gastric variceal hemorrhage or massive splenomegaly.
4. Addressing Underlying Causes
-
Pancreatic tumors or chronic inflammation must be concurrently treated.
Prognosis
-
Excellent for asymptomatic cases with conservative management.
-
Risk increases significantly with gastric variceal hemorrhage, which can be fatal if untreated.
-
Prognosis depends heavily on timely diagnosis and control of the underlying cause (e.g., pancreatitis or neoplasm).
Expert Radiology Quiz
Question 1
What is the most likely diagnosis based on the CT findings?
A. Inferior vena cava thrombosis
B. Splenic vein thrombosis
C. Superior mesenteric artery thrombosis
D. Hepatic artery thrombosis
Explanation: The CT image reveals a filling defect in the splenic vein in the setting of pancreatitis, classic for SVT.
Question 2
What is the most common complication of splenic vein thrombosis?
A. Hepatic encephalopathy
B. Portal vein thrombosis
C. Gastric varices
D. Ascites
Explanation: Collateral venous circulation due to SVT often leads to isolated gastric varices, which are prone to bleeding.
Question 3
Which condition most frequently causes splenic vein thrombosis?
A. Cirrhosis
B. Pancreatic cancer
C. Acute pancreatitis
D. Gallbladder stones
Explanation: Inflammatory processes from acute pancreatitis are the leading cause of SVT.
References
-
Butler JR et al. Natural history of pancreatitis-induced splenic vein thrombosis: a systematic review. J Gastrointest Surg. 2011;15(11):2023–2029.
-
Heider TR et al. Natural history of pancreatitis-induced splenic vein thrombosis. Ann Surg. 2004;239(6):876–880.
-
Gonzalez HJ et al. Splanchnic vein thrombosis in acute pancreatitis: institutional experience. HPB (Oxford). 2011;13(12):860–864.
-
Sakorafas GH et al. Sinistral portal hypertension in chronic pancreatitis. Am J Surg. 2000;179(2):129–133.
-
Shah PA et al. Management of splenic vein thrombosis: perspectives and protocols. Clin Exp Gastroenterol. 2019;12:213–223.
-
Amin S et al. Sinistral portal hypertension: imaging and management. J Clin Exp Hepatol. 2015;5(4):360–363.
-
Stawicki SP et al. Vascular complications of pancreatitis. J Gastrointest Surg. 2013;17(10):1857–1863.
Final Thoughts
Although splenic vein thrombosis may be underrecognized, especially in asymptomatic patients, its detection can prevent fatal complications such as gastric variceal bleeding. Radiologists and clinicians should maintain a high index of suspicion in pancreatitis patients, particularly when CT or MRI reveals venous abnormalities.




Comments
Post a Comment