CT Imaging in Proctitis: A Radiologic Insight
Author: Dr. H.Jae Lee, MD, PhD
Date: June 9, 2025
Category: Radiology | Gastroenterology | Clinical Imaging
Introduction
Proctitis refers to inflammation of the rectal mucosa and is a frequently encountered condition in both outpatient and emergency clinical settings. Though often considered a benign disease, proctitis can signal an underlying infectious, inflammatory, or ischemic pathology. Imaging, particularly computed tomography (CT), plays a crucial role in evaluating the extent of disease and identifying associated complications. This post analyzes a representative case of proctitis as seen on CT imaging and delves into the underlying causes, diagnostic features, and management strategies.
Case Summary (Adapted from SVUH Radiology)
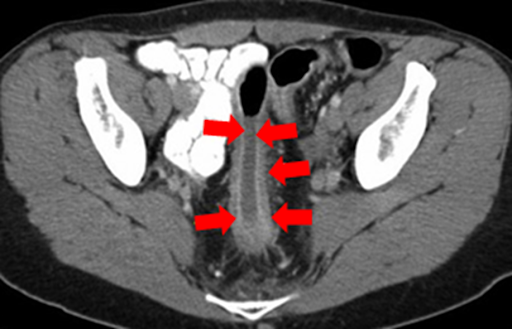
A patient presented with non-specific lower abdominal discomfort, urgency, and rectal pain. A contrast-enhanced CT abdomen and pelvis revealed circumferential mural thickening of the rectal wall with perirectal fat stranding and mucosal hyperenhancement, consistent with acute proctitis. No abscess formation or perforation was noted.
Discussion
Cause and Etiology
Proctitis may arise from a variety of etiologies, which can broadly be divided into the following categories:
-
Infectious: Common organisms include Neisseria gonorrhoeae, Chlamydia trachomatis, Herpes simplex virus (HSV), Treponema pallidum, and enteric pathogens such as Salmonella or Shigella. Sexually transmitted infections (STIs) are particularly common in men who have sex with men (MSM).
-
Inflammatory: Includes idiopathic inflammatory bowel disease (IBD), particularly ulcerative colitis and Crohn’s disease.
-
Radiation-induced: Frequently observed in patients receiving pelvic radiotherapy for prostate or gynecological cancers.
-
Ischemic: Often occurs in elderly patients with comorbid vascular disease.
-
Iatrogenic: Post-surgical, post-endoscopic, or following enema administration.
Pathophysiology
The pathogenesis varies by cause. In infectious proctitis, direct invasion of the rectal mucosa leads to inflammation, ulceration, and possibly abscess formation. In IBD, immune-mediated mechanisms result in chronic mucosal inflammation and disruption of the epithelial barrier. Ischemic proctitis results from reduced blood flow and tissue hypoxia, leading to mucosal necrosis.
Epidemiology
-
More prevalent in adults aged 20–50.
-
Higher incidence among individuals with risky sexual behaviors, particularly MSM.
-
Radiation proctitis has a reported incidence of 5–20% in patients receiving pelvic radiotherapy.
-
Ischemic proctitis remains rare due to the rectum’s robust collateral blood supply.
Clinical Presentation
Symptoms may include:
-
Tenesmus (painful urge to defecate)
-
Rectal bleeding
-
Mucopurulent discharge
-
Anal pain or discomfort
-
Diarrhea or constipation
Fever and systemic signs may suggest abscess formation or severe inflammation.
Imaging Features
CT findings of proctitis typically include:
-
Diffuse or segmental rectal wall thickening
-
Hyperenhancement of the mucosa
-
Perirectal fat stranding
-
Preserved or obliterated rectal lumen
-
Absence or presence of complications such as perforation, abscess, or fistula
MRI and endoscopy provide higher mucosal resolution, but CT remains valuable for acute assessment and excluding other pathologies.
Treatment
Management depends on the underlying cause:
-
Infectious: Targeted antibiotics or antivirals (e.g., ceftriaxone for gonorrhea, doxycycline for chlamydia).
-
Inflammatory: Aminosalicylates, corticosteroids, or biologics.
-
Radiation-induced: Sucralfate enemas, anti-inflammatory therapy, or hyperbaric oxygen.
-
Ischemic: Supportive care, bowel rest, and management of underlying vascular conditions.
Prognosis
-
Infectious and mild idiopathic cases often resolve with medical therapy.
-
Chronic inflammation, particularly in IBD or radiation-induced cases, may lead to fibrosis, strictures, or colorectal neoplasia.
-
Complicated cases with perforation or abscess carry a higher risk of morbidity.
References
-
Feuerstadt, P., Brandt, L. J. (2015). Ischemic proctitis: clinical features and management. American Journal of Gastroenterology, 110(5), 701–706. https://doi.org/10.1038/ajg.2015.93
-
Khan, M. A., Bhatnagar, G., Scarsbrook, A. F. (2013). Imaging in inflammatory bowel disease: CT and MRI. Clinical Radiology, 68(7), 705–714. https://doi.org/10.1016/j.crad.2013.02.008
-
Ghosh, S., Mitchell, R. (2020). Radiation proctitis: pathophysiology and modern management. Colorectal Disease, 22(1), 7–17. https://doi.org/10.1111/codi.14806
-
Quiles, A. M., Regueiro, M. D. (2015). Proctitis and perianal disease. Clinics in Colon and Rectal Surgery, 28(3), 130–137. https://doi.org/10.1055/s-0035-1554912
-
Owens, S. R., Greenson, J. K. (2007). Histopathology of IBD. Modern Pathology, 20(S1), S88–S98. https://doi.org/10.1038/modpathol.3800718
Quiz
1. Which of the following is not a typical cause of proctitis?
A. Gonorrhea
B. Ulcerative colitis
C. Appendicitis
D. Radiation therapy
Explanation: Appendicitis involves the appendix and does not typically cause proctitis. The other options are well-known causes of proctitis.
2. Which imaging feature is most characteristic of acute proctitis on CT?
A. Colonic diverticula
B. Air-fluid levels in the colon
C. Rectal wall thickening with mucosal enhancement
D. Normal rectal wall appearance
Explanation: This finding is a hallmark sign of inflammation in the rectum and strongly supports a diagnosis of proctitis.
Conclusion
CT imaging provides a valuable diagnostic tool in evaluating patients with rectal symptoms suggestive of proctitis. While endoscopy remains the gold standard for mucosal assessment, radiologic features can offer rapid, non-invasive insights, particularly in acute settings. Recognizing the diverse etiologies and imaging appearances of proctitis is essential for accurate diagnosis and management.
Comments
Post a Comment