Zinner syndrome
Zinner Syndrome Overview
Zinner syndrome is a rare congenital
malformation of the male genitourinary tract, characterized by the classic
triad of:
- Unilateral renal agenesis
- Ipsilateral seminal vesicle cyst
- Ejaculatory duct obstruction
It is considered the male
counterpart of the Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome in
females.
1. Cause and Etiology
Zinner syndrome results from abnormal
development of the mesonephric (Wolffian) duct during embryogenesis,
particularly between the 4th and 13th weeks of gestation.
- Mesonephric duct derivatives in males include:
- Epididymis
- Vas deferens
- Seminal vesicle
- Ejaculatory duct
- Trigone of the bladder
- Ureteric bud (which forms the ureter, renal pelvis,
calyces, and collecting ducts)
- In Zinner syndrome, there is maldevelopment or
failure of the ureteric bud to induce the metanephric blastema,
leading to unilateral renal agenesis. Simultaneously, the malformed
distal mesonephric duct contributes to seminal vesicle cyst formation
and ejaculatory duct obstruction.
2. Pathophysiology
- Renal Agenesis: Absence of one kidney
due to failed ureteric bud development.
- Seminal Vesicle Cyst: Because the ejaculatory
duct is obstructed or hypoplastic, secretions from the seminal vesicle
cannot be drained, leading to cystic dilatation.
- Ejaculatory Duct Obstruction: Impedes sperm and
seminal fluid passage during ejaculation, contributing to infertility and
sometimes pain.
The cysts may enlarge over
time, becoming symptomatic due to pressure effects or secondary infection.
3. Epidemiology
- Prevalence: Very rare; fewer than
300 cases reported in the literature.
- Sex: Occurs exclusively in males.
- Laterality: Usually affects the left
side more frequently.
- Age at presentation: Typically in the second
to fourth decades of life, often when patients seek evaluation for
infertility or pelvic pain.
- Asymptomatic cases: Some are detected
incidentally during imaging for unrelated reasons.
4. Clinical Presentation
Symptoms usually arise from
the enlarging seminal vesicle cyst and related obstruction. Common
presentations include:
- Lower urinary tract symptoms (LUTS):
- Dysuria
- Frequency
- Urgency
- Perineal discomfort
- Pain:
- Perineal or pelvic pain
- Painful ejaculation
- Sexual/Reproductive symptoms:
- Painful ejaculation
- Hematospermia
- Decreased ejaculate volume
- Infertility (often oligospermia or azoospermia)
- Infection:
- Recurrent urinary tract infections (UTIs)
- Prostatitis or seminal vesiculitis
In rare cases, large cysts may
cause:
- Compression of adjacent structures (e.g., bladder,
rectum)
- Obstructive uropathy of the contralateral kidney
5. Imaging Features
Imaging is crucial for
diagnosis. Modalities include:
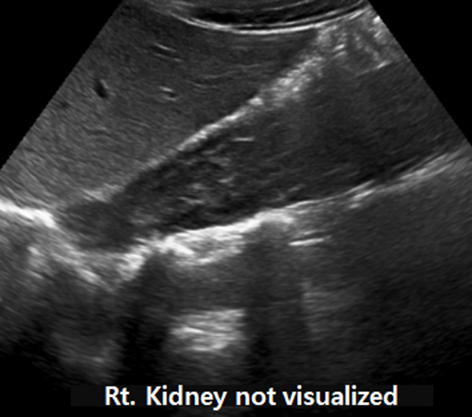
Ultrasound (US)
- May show:
- Absence of one kidney
- Cystic mass in the pelvis or retrovesical space
Computed Tomography (CT)
- Useful for:
- Confirming renal agenesis
- Visualizing seminal vesicle cyst
(well-defined, fluid-attenuation mass)
- Assessing mass effect on adjacent organs
Magnetic Resonance Imaging
(MRI)
https://doi.org/10.1038/s41443-020-00360-0
- Gold standard for diagnosis due to
superior soft tissue contrast
- Features:
- Seminal vesicle cyst: Hyperintense on
T2-weighted images
- Renal agenesis: Absence of renal
tissue in renal fossa
- No enhancement post-gadolinium unless infected
- Associated atrophic vas deferens or ejaculatory
duct can sometimes be visualized
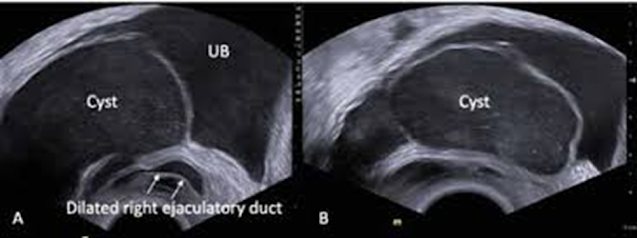
Transrectal Ultrasound (TRUS)
Transrectal sonography (TRUS) images showing dilated right
ejaculatory duct communicating with dilated right seminal vesicle protruding
into the urinary bladder (A); Rather than purely anechoic, there are
innumerable punctate echogenic dots/ low level internal echoes seen within the
cyst (B). https://doi.org/10.3126/jssn.v24i2.42837
- Useful for guiding aspiration or biopsy
- Helps assess communication with seminal vesicles
6. Treatment
Treatment is based on symptom
severity.
Asymptomatic patients:
- Observation with regular follow-up
imaging
Symptomatic patients:
- Medical treatment (limited role):
- Antibiotics for infection
- Analgesics for pain
Surgical treatment:
- Cyst aspiration (transrectal or
percutaneous): Temporary relief; high recurrence rate
- Transurethral resection of the ejaculatory duct
(TURED):
- Effective for drainage and symptom relief
- Can improve fertility outcomes
- Laparoscopic or robotic-assisted excision:
- Definitive treatment
- Preferred for large or recurrent cysts
- Allows removal of the entire cyst with minimal
morbidity
7. Prognosis
- Excellent prognosis with appropriate
treatment.
- Fertility may improve after relieving
ejaculatory duct obstruction.
- Rare complications:
- Recurrence of cysts (if not completely excised)
- Chronic pelvic pain (if untreated)
- Psychological distress from infertility
8. Differential Diagnosis
Other causes of pelvic cystic
lesions in men include:
- Müllerian duct cyst
- Prostatic utricle cyst
- Ejaculatory duct cyst (not associated with renal
agenesis)
- Abscess
- Hydatid cyst
- Cystic neoplasms
MRI and clinical correlation
are key to distinguishing Zinner syndrome.
Summary Table
|
Feature |
Zinner Syndrome |
|
Etiology |
Wolffian duct anomaly during
embryogenesis |
|
Triad |
Renal agenesis + seminal
vesicle cyst + ejaculatory duct obstruction |
|
Symptoms |
Pelvic pain, LUTS, painful
ejaculation, infertility |
|
Best Imaging |
MRI |
|
Treatment (Symptomatic) |
TURED, laparoscopic cyst
excision |
|
Prognosis |
Good, especially with
surgical treatment |
===============================================================
Case study: Elevated Creatinine Levels in a 68-Year-Old Man
Zinner Syndrome
History and Imaging Findings
-
This case involves a 68-year-old male patient diagnosed with stage IIIA chronic kidney disease (CKD), who has a congenitally absent left kidney.
-
He presented with resistant hypertension and elevated serum creatinine levels.
-
A computed tomography (CT) scan was performed.
Quiz:
-
Hydronephrosis is one of the most critical diagnoses to exclude in patients with elevated creatinine levels.
(1) True
(2) False
Explanation: In acute settings, hydronephrosis is among the most important conditions for patients with elevated creatinine levels. This is because urgent decompression can provide life-saving treatment. -
In a male patient with a congenitally absent kidney and infertility, which of the following structures is most likely to be affected?
(1) Ejaculatory duct
(2) Urethra
(3) Testis
(4) Rectum
(5) All of the above
Explanation: Male patients with a congenital absence of the kidney and infertility are likely to have ejaculatory duct obstruction, a hallmark feature of Zinner syndrome.
|
|
Zinner Syndrome is a rare congenital malformation characterized by the following key features. It arises from abnormalities in the mesonephric (Wolffian) duct and predominantly affects males. Key Features of Zinner Syndrome
Because these features often present with nonspecific symptoms such as abdominal pain or difficulty with urination, diagnosis can be challenging. Diagnosis and Treatment
|
3. According to the CT images, the left seminal vesicle is absent.
(1) True
(2) False
Explanation: The images show the presence of the bladder, right seminal vesicle, and rectum. However, the left seminal vesicle is absent.
Findings and Diagnosis
Findings:
There is congenital absence of the left kidney. Additionally, the left seminal vesicle is also absent.
Differential Diagnosis:
-
Müllerian agenesis
|
|
Key Features of Müllerian Agenesis
Symptoms
Diagnosis and Treatment
|
- Zinner Syndrome
Diagnosis: Zinner Syndrome
Discussion
Zinner Syndrome
Epidemiology and Pathogenesis
Congenital anomalies of the seminal vesicles are exceedingly rare. Because the ureteric bud and seminal vesicles both originate embryologically from the mesonephric (Wolffian) duct, abnormalities in this structure frequently result in associated defects in the ipsilateral upper urinary tract. The triad of a seminal vesicle cyst or agenesis, ipsilateral renal agenesis, and ejaculatory duct obstruction defines Zinner Syndrome. This syndrome results from mesonephric duct maldevelopment before the 7th week of gestation. It typically remains asymptomatic during childhood and becomes clinically apparent in the third or fourth decade of life.
Clinical Presentation
The clinical manifestations of Zinner Syndrome vary widely. However, patients often present with one or more of the following symptoms:
-
Dysuria
-
Infertility
-
Chronic pelvic pain
-
Painful ejaculation
-
Hematuria
-
Lower urinary tract symptoms (LUTS)
-
Urinary tract infections (UTIs)
Imaging Findings
Radiologic features suggestive of Zinner Syndrome typically include:
-
Ipsilateral congenital renal agenesis
-
Seminal vesicle cyst or agenesis on the affected side
-
Ejaculatory duct obstruction
Additional findings may include:
-
Small testis
-
Ipsilateral ureterocele
Treatment
Management of symptomatic patients often involves surgical excision of the seminal vesicle cyst. In patients with infertility, transurethral resection of the ejaculatory duct (TURED) may be indicated. For those with bilateral renal hypoplasia or agenesis, renal replacement therapy may be required.
References
-
Ibrahim D. Zinner syndrome: Radiology Reference Article. Radiopaedia. https://radiopaedia.org/articles/zinner-syndrome-1.
-
Talwar HS, Mittal A, Narain TA, Panwar VK. A wide spectrum of rare clinical variants of Zinner syndrome. BMJ Case Reports CP. 2021;14(1):e239254. doi:10.1136/bcr-2020-239254.





Comments
Post a Comment