Subchondral Insufficiency Fracture of the Knee: A Hidden Culprit of Joint Pain in Elderly Women
Introduction
Knee
pain in elderly individuals is often attributed to degenerative joint disease,
such as osteoarthritis. However, when the pain is sudden, severe, and worsened
by weight-bearing, particularly in older women without significant trauma
history, a more elusive diagnosis must be considered: Subchondral Insufficiency
Fracture (SIF).
In
this article, we present a case of SIF in a 66-year-old woman, utilizing multimodal imaging, and provide an in-depth review of its clinical implications,
MRI findings, differential diagnosis, treatment options, and prognosis.
Case
Summary
Patient:
66-year-old female
Chief
complaint: Acute knee pain after minor twisting injury
Pain:
Sharp, worsened by movement and weight-bearing
Imaging:
Plain radiographs and MRI
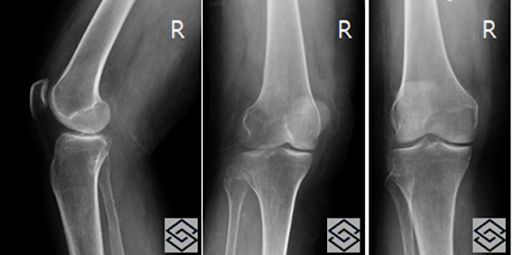
Radiographic Findings
Subtle
sclerosis in the medial femoral condyle
No
clear fracture line or collapse
Mild
joint effusion
Radiographs
were inconclusive, prompting further imaging with MRI.
MRI Findings
Curvilinear
hypointense line along the subchondral surface of the medial femoral condyle
(low signal on T1 and PD-FS)
Extensive
surrounding bone marrow edema
Subchondral
fluid-filled cleft indicating possible cortical collapse
Full-thickness
cartilage loss
Extrusion
of the medial meniscus
Subchondral
fracture was also noted in the medial tibial plateau
Partial
tear of the medial collateral ligament (MCL)
Quiz
1.
Which component has a subtle finding that may require further workup?
(A)
Inferior patellar border
(B)
Medial femoral condyle
(C)
Medial femoral epicondyle
(D)
Tibial tuberosity
(E)
Quadriceps tendon
Explanation:
Subtle sclerosis in the medial femoral condyle may suggest a subchondral
insufficiency fracture. Further MRI workup is warranted if symptoms are severe.
2.
There is a curvilinear low signal along the subchondral medial femoral condyle.
(A) TRUE
(B)
FALSE
Explanation: This finding is classic for subchondral fracture—a low-signal intensity line representing cortical discontinuity.
3.
Which of the following is a poor prognostic indicator in subchondral
insufficiency fracture?
(A)
Extensive bone marrow edema
(B)
Medial meniscus extrusion
(C)
Subchondral hypointense line > 1 cm
(D)
Subchondral fluid-filled cleft
(E) All
of the above
Explanation:
A longer hypointense line, extrusion of meniscus, and subchondral fluid cleft
all suggest subchondral plate collapse, which correlates with poor prognosis.
Discussion
Cause & Etiology
Subchondral
insufficiency fracture (SIF) occurs when normal mechanical stress exceeds the
structural integrity of osteopenic or osteoporotic subchondral bone. It is more
common in elderly women, often without trauma.
Key
risk factors: Osteoporosis, advanced age, varus/valgus alignment, repetitive
microtrauma, post-menopausal bone loss.
Pathophysiology
Weight-bearing
causes microfractures in the subchondral plate.
Inadequate
repair → collapse of the subchondral bone
Joint
surface becomes unstable → leads to cartilage degeneration
In chronic stages, it may mimic or evolve into osteoarthritis or osteonecrosis
Epidemiology
More
prevalent in women > 60 years
Often
underdiagnosed due to nonspecific radiographic findings
May coexist with meniscal extrusion or partial MCL injuries
Imaging Features
|
Modality |
Key Findings |
|
X-ray |
Often
normal or subtle sclerosis |
|
MRI |
Curvilinear
hypointense subchondral line
Bone
marrow edema
Cartilage
loss
Meniscal
extrusion
Joint
effusion
Subchondral
fluid cleft
Possible
secondary tibial plateau involvement
Differential Diagnosis
Osteochondral
impaction fracture
Avascular
necrosis (AVN)
Transient
bone marrow edema syndrome
Osteoarthritis
Meniscal
root tears
Key
distinction:
SIF presents with acute pain and MRI evidence of subchondral fracture without
systemic bone infarction, differentiating it from AVN.
Treatment
Conservative
management (if early-stage):
Non-weight-bearing
with crutches
NSAIDs
Bisphosphonates
(controversial)
Physical
therapy
Surgical
management (if collapse or non-responsive):
Core
decompression
Subchondroplasty
High
tibial osteotomy (HTO)
Partial
or total knee arthroplasty (TKA)
Prognosis
Early
diagnosis is key to preventing joint collapse
Lesions
with fluid-filled clefts or >1 cm fracture lines are associated with poor
outcomes
Meniscal
extrusion and full-thickness cartilage loss worsen prognosis
Progression to osteoarthritis is common if untreated
Conclusion
Subchondral
insufficiency fracture is an under-recognized but significant cause of knee
pain, especially in elderly women. Careful clinical suspicion and MRI
interpretation are crucial for distinguishing SIF from arthritis or
osteonecrosis. Early diagnosis can change the trajectory of care, preventing
irreversible joint collapse and disability.
References
[1]
R. Yamamoto and M. Bullough, "Osteonecrosis: Diagnosis and
management," J. Bone Joint Surg. Am., vol. 82, no. 3, pp. 377–387,
Mar. 2000.
[2]
T. Chiba et al., "Subchondral insufficiency fracture of the femoral
head," Clin Orthop Relat Res., vol. 399, pp. 145–153, 2002.
[3]
A. T. Carrino et al., "MRI of subchondral insufficiency fractures of the
knee," Radiology, vol. 237, no. 3, pp. 998–1007, Dec. 2005.
[4]
H. Yamagami et al., "Subchondral insufficiency fracture of the knee:
Imaging features and treatment outcomes," Radiographics, vol. 33,
no. 1, pp. 139–155, Jan. 2013.
[5] E. A. Schweitzer, "MRI of knee cartilage and subchondral bone: Pathologies and pitfalls," Am J Roentgenol, vol. 200, no. 3, pp. 555–564, Mar. 2013.

Comments
Post a Comment