Preseptal Cellulitis
1. Definition
Preseptal cellulitis (also called periorbital cellulitis) is an infection of the subcutaneous tissues anterior to the orbital septum, which includes the eyelid, periorbital skin, and subcutaneous tissues, but not the orbit itself. It must be distinguished clinically and radiologically from orbital cellulitis, which involves infection posterior to the orbital septum and carries a significantly higher risk of complications, including vision loss and intracranial spread.
2. Etiology and Causes
2.1. Etiologic Agents
Preseptal cellulitis is usually caused by bacterial pathogens. The most common organisms include:
-
Staphylococcus aureus (including MRSA)
-
Streptococcus pyogenes (Group A Streptococcus)
-
Streptococcus pneumoniae
-
Haemophilus influenzae type B (Hib) – historically important, especially in children before widespread vaccination
2.2. Routes of Infection
-
Contiguous spread from adjacent structures:
-
Sinusitis (especially ethmoid and maxillary)
-
Hordeolum (stye), chalazion
-
Infected insect bite or trauma
-
Skin infection, such as impetigo or facial cellulitis
-
-
Hematogenous spread: Rare, may occur in bacteremia, especially in children
-
Iatrogenic causes: Following surgical procedures, cosmetic injections, or dental work
3. Pathophysiology
Preseptal cellulitis arises when pathogenic bacteria breach the cutaneous or mucosal barrier of the periorbital skin. The bacteria proliferate within the loose connective tissue, producing localized inflammation characterized by:
-
Vasodilation
-
Capillary leak
-
Edema
-
Neutrophil infiltration
-
Cytokine-mediated tissue responses (IL-1, IL-6, TNF-α)
This leads to swelling, erythema, and warmth of the eyelid and periorbital area. Unlike orbital cellulitis, there is no involvement of orbital fat, muscles, or optic nerve, and hence no impairment of extraocular motion or vision.
4. Epidemiology
4.1. Age and Demographics
-
Most common in children, particularly those under 5 years of age
-
Less common but still occurs in adults, often due to trauma or skin infection
4.2. Incidence and Trends
-
Widespread Hib vaccination has significantly reduced the incidence in children
-
Incidence is approximately 5–10 cases per 100,000 per year in children
-
Slight male predominance reported
4.3. Risk Factors
-
Sinus infections
-
Skin trauma or insect bites near the eyes
-
Immunosuppression (diabetes, cancer, HIV)
-
Recent upper respiratory infections
5. Clinical Features
5.1. Symptoms
-
Eyelid swelling
-
Erythema and warmth of the eyelid/periorbital skin
-
Tenderness on palpation
-
Eyelid induration
-
Low-grade fever (may be absent)
-
Malaise
5.2. Signs That Suggest Orbital Involvement (Red Flags)
If any of the following are present, consider orbital cellulitis or another orbital pathology:
-
Proptosis
-
Pain with eye movements
-
Ophthalmoplegia or limited extraocular movements
-
Decreased visual acuity
-
Afferent pupillary defect
-
Chemosis (conjunctival edema)
6. Imaging Findings
-
Diagnosis is uncertain
-
Orbital involvement is suspected
-
Symptoms do not improve with treatment
-
Severe symptoms are present
-
There is a history of trauma or a foreign body
6.1. Preferred Imaging Modality: Contrast-enhanced CT of the orbits and sinuses
Findings in Preseptal Cellulitis:
-
Inflammation and fat stranding are confined anterior to the orbital septum
-
No involvement of the orbital fat, extraocular muscles, or globe
-
No proptosis
-
Sinusitis may be present as a source
-
6.2. MRI
Rarely used, but better for evaluating complications such as cavernous sinus thrombosis or intracranial extension
7. Treatment
7.1. General Approach
-
Empirical antibiotic therapy based on likely organisms
-
Outpatient management if the patient is non-toxic and orbital cellulitis is excluded
-
Inpatient management is:
-
A child is <1 year old
-
Severe symptoms
-
Immunocompromised state
-
Suspicion of orbital extension
-
7.2. Antibiotics
Outpatient (Oral antibiotics):
-
Amoxicillin-clavulanate
-
Cephalexin
-
Clindamycin or TMP-SMX (if MRSA is suspected) in combination with coverage for Streptococcus (e.g., amoxicillin)
Inpatient (IV antibiotics):
-
Ampicillin-sulbactam or ceftriaxone + clindamycin
-
Vancomycin if MRSA is a concern
7.3. Supportive Measures
-
Warm compresses
-
Analgesics
-
Antipyretics
-
Monitoring for signs of orbital involvement
7.4. Surgical Intervention
-
Rare in preseptal cellulitis alone
-
Indicated only if an abscess forms or orbital cellulitis develops
8. Differential Diagnosis
-
Orbital cellulitis
-
Allergic periorbital edema (e.g., contact dermatitis)
-
Herpes zoster ophthalmicus
-
Traumatic eyelid hematoma
-
Nephrotic syndrome (causing periorbital edema)
-
Blepharitis or conjunctivitis
9. Complications
While preseptal cellulitis is typically benign and self-limited with treatment, potential complications include:
-
Progression to orbital cellulitis
-
Formation of subperiosteal or orbital abscess
-
Vision loss (if not treated and progresses)
-
Cavernous sinus thrombosis (rare, life-threatening)
-
Septicemia, especially in infants or immunocompromised
10. Prognosis
-
Excellent with prompt diagnosis and treatment
-
Most cases resolve within 5–7 days
-
No long-term sequelae in the majority of cases
-
Poor outcome is more likely in:
-
Delayed treatment
-
Misdiagnosis as orbital cellulitis
-
Immunocompromised individuals
-
Case study: A 6-year-old girl presents with a 2-day history of progressive swelling and redness of the left upper eyelid
1. History and Images
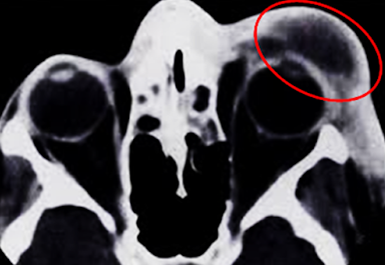
A 6-year-old girl presents with a 2-day history of progressive swelling and redness of the left upper eyelid. No trauma is recalled, but the patient had a recent upper respiratory tract infection. She has a mild fever (38.2°C), no visual complaints, and no pain with eye movements. On examination, her vision and extraocular muscle function are intact. There is no proptosis or chemosis.
Imaging Interpretation
-
Marked preseptal soft tissue swelling in the left upper eyelid
-
Fat stranding limited to the anterior orbital region, without breach of the orbital septum
-
No proptosis, extraocular muscle enlargement, or orbital fat infiltration
-
No sinus opacification or signs of orbital abscess
Diagnosis: Preseptal cellulitis (confirmed by absence of postseptal involvement)
Question
Which CT feature best helps differentiate preseptal from orbital cellulitis?
Correct Answer: C. Absence of postseptal fat stranding
Explanation:
-
Preseptal cellulitis is limited to the anterior compartment of the orbit and does not extend beyond the orbital septum.
-
CT showing inflammation confined anterior to the orbital septum, without orbital fat stranding or extraocular muscle involvement, confirms preseptal over orbital cellulitis.
-
Sinus opacification and conjunctival changes may be present in either condition.
Preseptal cellulitis is limited to the anterior compartment of the orbit and does not extend beyond the orbital septum.
CT showing inflammation confined anterior to the orbital septum, without orbital fat stranding or extraocular muscle involvement, confirms preseptal over orbital cellulitis.
Sinus opacification and conjunctival changes may be present in either condition.
3. Discussion
Pathophysiology
Preseptal cellulitis is an acute infection localized to the eyelid and periorbital soft tissues anterior to the orbital septum. It may arise via:
-
Contiguous spread from local infections (e.g., hordeolum, impetigo, sinusitis)
-
Trauma or insect bites
-
Hematogenous spread in systemic infections
The orbital septum, a fibrous membrane arising from the orbital rim, acts as a barrier that prevents posterior spread. If this barrier is breached, infection may progress to orbital cellulitis or even subperiosteal abscess.
Epidemiology
-
Most commonly affects children <10 years
-
Increased risk with URI, sinus infections, and skin trauma
-
Incidence significantly decreased post-introduction of the Hib vaccine
Most commonly affects children <10 years
Increased risk with URI, sinus infections, and skin trauma
Incidence significantly decreased post-introduction of the Hib vaccine
Clinical Presentation
-
Periorbital edema, erythema, and tenderness
-
No visual impairment, no pain on eye movement
-
May have a low-grade fever
-
Absence of: proptosis, ophthalmoplegia, chemosis, decreased acuity
Periorbital edema, erythema, and tenderness
No visual impairment, no pain on eye movement
May have a low-grade fever
Absence of: proptosis, ophthalmoplegia, chemosis, decreased acuity
Imaging Features
-
CT with IV contrast is ideal for:
-
Delineating preseptal vs orbital involvement
-
Detecting complications (e.g., abscess, sinusitis)
-
Preseptal Cellulitis CT findings:
-
Anterior soft tissue swelling
-
No orbital fat stranding or muscle enlargement
-
No sinus involvement (optional finding)
-
MRI is reserved for equivocal cases or suspected intracranial extension
CT with IV contrast is ideal for:
-
Delineating preseptal vs orbital involvement
-
Detecting complications (e.g., abscess, sinusitis)
Preseptal Cellulitis CT findings:
-
Anterior soft tissue swelling
-
No orbital fat stranding or muscle enlargement
-
No sinus involvement (optional finding)
MRI is reserved for equivocal cases or suspected intracranial extension
Treatment
-
Mild/moderate cases:
-
Empiric oral antibiotics: e.g., amoxicillin-clavulanate
-
Moderate/severe cases or age <1 year:
-
IV antibiotics: e.g., ceftriaxone, vancomycin if MRSA suspected
-
Supportive: Warm compresses, hydration, fever control
Mild/moderate cases:
-
Empiric oral antibiotics: e.g., amoxicillin-clavulanate
Moderate/severe cases or age <1 year:
-
IV antibiotics: e.g., ceftriaxone, vancomycin if MRSA suspected
Supportive: Warm compresses, hydration, fever control
Prognosis
-
Excellent with timely intervention
-
Resolution is typically within 5–7 days
-
Close follow-up is essential to monitor for progression
-
Rare complications: abscess formation, orbital cellulitis, vision loss (if untreated)
Excellent with timely intervention
Resolution is typically within 5–7 days
Close follow-up is essential to monitor for progression
Rare complications: abscess formation, orbital cellulitis, vision loss (if untreated)
References
-
Baring DE, et al. Management of periorbital and orbital cellulitis. J Laryngol Otol. 2007;121(4):326–328.
-
Tiu CM, et al. Preseptal and orbital cellulitis: Imaging features and clinical differentiation. AJR Am J Roentgenol. 1999;173(3):667–672.
-
Wald ER. Periorbital and Orbital Infections. Pediatr Rev. 2004;25(9):312–319.
-
McKinley SH, et al. Comparison of contrast-enhanced CT and MRI in evaluating orbital infections. Radiographics. 2003;23(1):179–190.
-
American Academy of Pediatrics. Red Book: 2021 Report of the Committee on Infectious Diseases.
Baring DE, et al. Management of periorbital and orbital cellulitis. J Laryngol Otol. 2007;121(4):326–328.
Tiu CM, et al. Preseptal and orbital cellulitis: Imaging features and clinical differentiation. AJR Am J Roentgenol. 1999;173(3):667–672.
Wald ER. Periorbital and Orbital Infections. Pediatr Rev. 2004;25(9):312–319.
McKinley SH, et al. Comparison of contrast-enhanced CT and MRI in evaluating orbital infections. Radiographics. 2003;23(1):179–190.
American Academy of Pediatrics. Red Book: 2021 Report of the Committee on Infectious Diseases.


Comments
Post a Comment