Paranasal Sinusitis: Overview
Paranasal sinusitis, also known simply as sinusitis, is an inflammation of the paranasal sinuses, which are air-filled spaces located within the bones of the skull and face. The condition can be acute, subacute, chronic, or recurrent, depending on the duration and frequency of episodes.
1. Cause and Etiology
Sinusitis occurs when the paranasal sinuses become inflamed or infected. This inflammation can result from a variety of causes, including:
-
Infections:
-
Viral infections: These are the most common cause, often following upper respiratory viral infections like the common cold.
-
Bacterial infections: Secondary bacterial infections may develop following viral sinusitis. The most common bacterial pathogens include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis.
-
Fungal infections: These are rare but may occur in immunocompromised individuals (e.g., patients with diabetes or those on immunosuppressive medications). Fungal species like Aspergillus can lead to invasive fungal sinusitis.
-
-
Allergic reactions: Allergic rhinitis can contribute to sinus inflammation, leading to sinusitis.
-
Anatomical issues: Structural abnormalities like a deviated septum, nasal polyps, or concha bullosa (enlarged middle turbinate) can obstruct sinus drainage and predispose to sinus infections.
-
Environmental factors: Exposure to irritants such as smoke, pollution, and allergens can increase the risk of developing sinusitis.
2. Pathophysiology
The paranasal sinuses are normally lined with mucous membranes that help to clear mucus and other debris. When the drainage pathways of the sinuses become blocked due to inflammation, the mucus accumulates, creating an environment conducive to bacterial or viral growth.
-
Obstruction of the sinus ostia: The primary pathophysiological mechanism in sinusitis is the obstruction of the sinus ostia, which are the natural openings that allow drainage of mucus. This obstruction can be caused by swelling of the mucosa, mechanical blockage (e.g., from nasal polyps or deviated septum), or excessive mucus production.
-
Mucosal inflammation: The blockage leads to mucosal inflammation, increased vascular permeability, and the accumulation of inflammatory cells within the sinuses. This results in the symptoms of sinusitis, including pain, pressure, and nasal congestion.
-
Bacterial or viral infection: Once the sinuses are obstructed and mucus accumulates, bacterial or viral pathogens can proliferate, leading to an infection.
3. Epidemiology
Sinusitis is a common condition, with a prevalence of up to 15% of adults in the general population experiencing it annually. Acute sinusitis is particularly common after viral upper respiratory infections. Chronic sinusitis affects approximately 12% of adults and is more common in individuals with allergies or structural nasal abnormalities.
-
Age and gender: Sinusitis can affect individuals of all ages. Acute sinusitis is most common in children and young adults, while chronic sinusitis tends to be more prevalent in middle-aged adults.
-
Risk factors: Certain factors increase the risk of sinusitis, including:
-
Nasal allergies (rhinitis)
-
Asthma
-
Smoking and exposure to second-hand smoke
-
Immunocompromised states (e.g., diabetes, HIV/AIDS)
-
Frequent respiratory infections
-
4. Clinical Presentation
The clinical presentation of sinusitis can vary depending on whether the condition is acute or chronic.
Acute Sinusitis:
-
Duration: Symptoms last for less than 4 weeks.
-
Symptoms:
-
Nasal congestion and obstruction
-
Purulent nasal discharge (yellow or green)
-
Facial pain or pressure, particularly around the eyes, forehead, or cheeks
-
Headache
-
Cough, especially at night
-
Fever (in cases of bacterial infection)
-
Reduced sense of smell (anosmia)
-
Chronic Sinusitis:
-
Duration: Symptoms persist for more than 12 weeks despite medical treatment.
-
Symptoms:
-
Persistent nasal congestion
-
Thick nasal discharge
-
Postnasal drip (drainage of mucus from the sinuses into the throat)
-
Facial pressure or fullness
-
Fatigue
-
Chronic cough
-
Hyposmia or anosmia
-
Possible dental pain (particularly with maxillary sinus involvement)
-
5. Imaging Features
The diagnosis of sinusitis is primarily clinical, but imaging studies can help confirm the diagnosis, assess the extent of disease, and rule out complications.
-
X-ray: Plain radiographs of the sinuses can be used, but they are not highly sensitive or specific. They can show sinus opacification or fluid levels, which may suggest sinusitis.
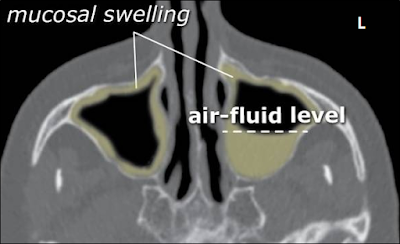
CT Scan: This is the gold standard for diagnosing sinusitis and evaluating the extent of sinus involvement. A CT scan of the sinuses can reveal mucosal thickening, sinus opacification, and obstructed sinus ostia. It is particularly helpful in chronic cases or when complications (e.g., abscess formation) are suspected.
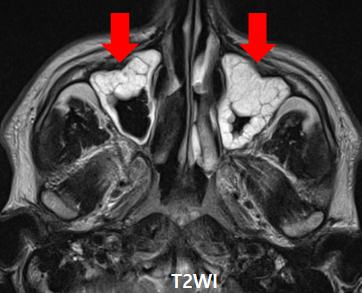
MRI: MRI is not typically used for routine diagnosis but can be helpful in assessing complications such as orbital or intracranial involvement. MRI provides superior soft tissue contrast but may not show bone involvement as well as CT.
6. Treatment
The treatment of sinusitis depends on its cause and severity, with the main goals being to relieve symptoms, treat the underlying infection, and prevent complications.
Acute Sinusitis:
-
Supportive care:
-
Decongestants (oral or nasal): These help to reduce nasal congestion and improve sinus drainage. However, nasal decongestant sprays should be used for no more than 3 days to avoid rebound congestion.
-
Saline nasal irrigation: This can help clear mucus from the sinuses and relieve congestion.
-
Analgesics/Antipyretics: Over-the-counter medications like acetaminophen or ibuprofen can help relieve pain and fever.
-
-
Antibiotics:
-
Indications for antibiotics: Antibiotics are recommended if symptoms persist for more than 10 days, worsen after an initial improvement, or if there is a high fever or severe facial pain.
-
First-line antibiotics: Amoxicillin or amoxicillin-clavulanate is commonly used.
-
Alternative antibiotics: For penicillin-allergic patients, doxycycline or a respiratory fluoroquinolone (e.g., levofloxacin) can be used.
-
Chronic Sinusitis:
-
Intranasal corticosteroids: These are the mainstay for managing chronic sinusitis, helping to reduce mucosal inflammation and promote drainage.
-
Nasal saline irrigation: Regular saline irrigation can help clear mucus and allergens from the nasal passages.
-
Antibiotics: In cases of chronic bacterial infection, a longer course of antibiotics may be required, often guided by culture results.
-
Surgery: In cases of refractory chronic sinusitis, surgical intervention (e.g., functional endoscopic sinus surgery, FESS) may be needed to remove obstructions, such as nasal polyps, and improve sinus drainage.
7. Prognosis
-
Acute Sinusitis: The prognosis for acute sinusitis is generally good. Most cases improve within 7 to 10 days with conservative treatment. However, bacterial infections may require antibiotics, and complications (e.g., abscess, orbital cellulitis) are rare but possible.
-
Chronic Sinusitis: Chronic sinusitis can be more challenging to treat and may require long-term management. Surgery may be necessary for individuals who do not respond to medical therapy. With appropriate treatment, many individuals with chronic sinusitis can achieve significant symptom relief, although some may experience recurrent episodes.
In conclusion, paranasal sinusitis is a common condition with a wide range of causes, from viral infections to allergic reactions and anatomical abnormalities. With early diagnosis and appropriate treatment, most cases can be managed effectively, but chronic or recurrent cases may require long-term therapy or surgery.
====================================
Case Study: A 15-year-old girl presented with a headache and chronic nasal congestion. Paranasal Sinusitis
History and Images
1. A 15-year-old girl presented with a headache and chronic nasal congestion
2. A CT coronal section through the paranasal sinuses was obtained.
3. Normal imaging and comparison images are presented.
1. Both ethmoid and maxillary sinus mucosa are thickened (arrow).2. This is a case of pansinusitis.
3. In cases of sinusitis, the scanning range should be set to encompass the entire sinus.
4. The degree of pneumatization of the frontal sinuses varies greatly among individuals.
Quiz:
1. Which of the following findings is most consistent with a diagnosis of pansinusitis on a CT scan?
A) Isolated mucosal thickening in the right maxillary sinus
B) Fluid level in the sphenoid sinus only
C) Mucosal thickening in both ethmoid and maxillary sinuses
D) Mucosal thickening and opacification in all paranasal sinuses
Correct Answer:
D) Mucosal thickening and opacification in all paranasal sinuses
Explanation:
Pansinusitis refers to the inflammation of all paranasal sinuses. While findings such as mucosal thickening in one or two sinuses (choices A and C) or a fluid level in a single sinus (choice B) may suggest localized sinusitis, only diffuse involvement of all sinuses supports a diagnosis of pansinusitis.
2. Why is it important to include the entire paranasal sinus region in the CT scan range when evaluating sinusitis?
A) To reduce radiation exposure
B) Because only the maxillary sinuses are clinically relevant
C) To ensure accurate assessment of the extent and severity of the disease
D) To avoid patient discomfort during the scan
Correct Answer:
C) To ensure accurate assessment of the extent and severity of the disease
Explanation:
A complete scan of the paranasal sinuses is essential in sinusitis cases to identify which sinuses are involved, detect complications, and plan appropriate treatment. Limited scanning may miss clinically significant findings, especially in cases like pansinusitis, where multiple sinuses are affected.


Comments
Post a Comment