Emphysematous Vertebral Osteomyelitis and Epidural Abscess Caused by Disseminated Klebsiella Infection
Emphysematous Vertebral Osteomyelitis and Epidural Abscess Caused by Disseminated Klebsiella Infection
1. Cause
and Etiology
Causative Organism:
·
Klebsiella pneumoniae is a
Gram-negative, encapsulated, facultatively anaerobic bacillus in the family
Enterobacteriaceae.
·
Hypervirulent strains, especially Klebsiella pneumoniae serotypes K1 and K2, are
increasingly associated with disseminated infections, including liver abscess,
endophthalmitis, meningitis, and spinal infections.
Routes of Infection:
·
Hematogenous spread from a primary
focus, typically from:
o
Pyogenic liver abscess (especially in
diabetics)
o
Urinary tract infections
o
Pneumonia
·
Rarely, direct inoculation or contiguous
spread from adjacent structures.
Risk Factors:
·
Diabetes mellitus (strongest risk
factor)
·
Immunosuppression (e.g., malignancy,
steroid use)
·
Chronic kidney disease
·
Advanced age
·
Alcohol use disorder
·
Asian ethnicity (hypervirulent strains are more prevalent in East Asia)
2. Pathophysiology
·
Dissemination:
Hypervirulent Klebsiella strains have
enhanced ability to invade tissues and evade host immune response, often
leading to metastatic infections.
·
Gas Production:
Emphysematous changes occur due to:
o
Bacterial fermentation of glucose and
tissue substrates under anaerobic or hypoxic conditions.
o
Production of hydrogen and carbon
dioxide gases.
·
Spinal Involvement:
o
Infection localizes to the vertebral
body via Batson’s plexus or arterial seeding.
o
Inflammatory destruction of bone and
intervertebral disc (discitis-osteomyelitis).
o
Extension to the epidural space forming an abscess.
o
Gas accumulation may occur in the
vertebrae, paraspinal soft tissues, or epidural space.
3. Epidemiology
·
Incidence: Emphysematous
vertebral osteomyelitis is rare, with only sporadic case reports.
·
Demographics:
o
Most patients are middle-aged to
elderly.
o
Males are slightly more affected.
o
High prevalence of diabetes in affected
individuals (>70% in case series).
·
Geography: More
frequently reported in East Asia, particularly Taiwan, South Korea, and Japan.
4. Clinical Presentation
Onset:
·
Subacute to acute, often over days to
weeks.
Symptoms:
·
Severe localized back pain (most common
symptom)
·
Fever and chills
·
Neurological deficits (radiculopathy,
paraparesis, or paraplegia due to cord compression)
·
Constitutional symptoms (weight loss,
malaise)
Signs:
·
Tenderness over affected spinal levels
·
Limited spinal motion
·
Neurological signs (depending on the extent
of the epidural abscess)
·
Possible signs of systemic infection
(sepsis, altered mental status)
Associated findings:
·
Hepatic abscess (especially in
hypervirulent Klebsiella infection)
·
Metastatic septic emboli (lungs, brain,
eye)
5. Imaging Features
A. CT Scan
·
Gas:
Hypodense areas within vertebral bodies or discs representing intraosseous gas.
·
Bone destruction:
Endplate erosion, lytic lesions.
·
Soft tissue involvement:
Paravertebral or psoas muscle abscesses.
·
Epidural abscess: May
show as a hypoattenuating collection with mass effect.
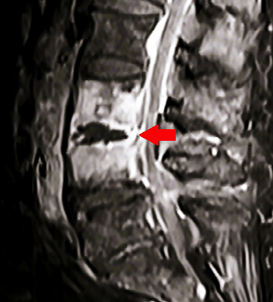
B. MRI (Gold standard
for spinal infection)
·
T1-weighted:
Hypointense vertebral body and disc signal.
·
T2-weighted/STIR:
Hyperintense vertebral bodies, disc, and paraspinal soft tissues.
·
Contrast-enhanced:
o
Rim-enhancing epidural abscess.
o
Enhancement of vertebral bodies and
disc.
·
Epidural space:
Compression of thecal sac or spinal cord.
C. X-ray (less
sensitive, late findings):
·
Vertebral collapse
·
Disc space narrowing
·
Gas (rarely seen)
6. Treatment
A. Medical Management
·
Antibiotics:
o
Empiric: Broad-spectrum IV antibiotics
targeting Gram-negative and anaerobic bacteria (e.g., cefepime + metronidazole
or meropenem).
o
Tailored therapy: Based on culture and
sensitivity (ESBL-producing strains may require carbapenems).
o
Duration: Typically 6–12 weeks of IV
antibiotics.
B. Surgical Management
·
Indicated for:
o
Neurological compromise (e.g., epidural
abscess with cord compression)
o
Spinal instability
o
Poor response to medical treatment
o
Large abscesses
·
Procedures:
o
Decompressive laminectomy and drainage
o
Corpectomy and spinal stabilization (if
needed)
C. Adjunctive Management
·
Glycemic control in diabetics
·
Management of primary infection source
(e.g., liver abscess drainage)
·
Supportive care: Pain control, bracing,
rehabilitation
7. Prognosis
Determinants of Outcome:
·
Early diagnosis and treatment
·
Presence of neurological deficits at
presentation
·
Control of primary infection source
·
Underlying comorbidities (especially
diabetes)
Outcomes:
·
With timely intervention, many patients
recover without permanent neurologic deficit.
·
Mortality can be high in cases with
delayed treatment or widespread sepsis.
·
Risk of recurrence or chronic
osteomyelitis if not adequately treated.
Summary Table
|
Category |
Details |
|
Organism |
Klebsiella pneumoniae (often hypervirulent strains) |
|
Risk Factors |
Diabetes,
immunosuppression, liver abscess |
|
Route |
Hematogenous spread |
|
Symptoms |
Back pain, fever,
neurologic deficits |
|
Imaging |
Gas in
vertebrae/disc/epidural space (CT/MRI), bone destruction |
|
Treatment |
IV antibiotics (6–12
weeks), surgical drainage if needed |
|
Prognosis |
Good with early
treatment; worsens with delayed care or sepsis |
References
1. Lee CH,
et al. Klebsiella
pneumoniae Spinal Epidural Abscess Associated with Liver Abscess. Infection. 2012.
2. Fang
CT, et al. Klebsiella pneumoniae genotype K1: An emerging
pathogen in invasive infections. Clin Infect
Dis. 2004.
3. Kim YJ,
et al. Emphysematous vertebral osteomyelitis: Report of
two cases. Spine J. 2010.
4. Sonneville
R, et al. Bacterial spinal epidural abscess. Lancet Infect Dis. 2017.
5. Wu MH, et al. Klebsiella pneumoniae liver abscess associated with metastatic endophthalmitis. Arch Intern Med. 2007.

Comments
Post a Comment