Pseudoaneurysm After Femoral Fracture
A pseudoaneurysm (false aneurysm) following a femoral fracture is a rare but
serious vascular complication.
1. Cause
A pseudoaneurysm occurs when
there is a breach in the arterial wall, leading to blood leakage that is
contained by the surrounding tissue, forming a pulsatile hematoma with a
fibrous capsule.
After a femoral fracture, this typically results from:
- Direct trauma from the fracture fragments to the femoral
artery (most often the superficial femoral artery).
- Iatrogenic injury during fracture fixation (e.g.,
intramedullary nailing, external fixation, or plate placement).
- Penetrating trauma or high-energy blunt trauma.
2. Etiology
- Blunt trauma (e.g., road traffic
accidents) causing sharp bone edges to lacerate or puncture the artery.
- Iatrogenic injury during orthopedic
surgical procedures.
- Penetrating trauma in open fractures.
- Delayed vascular injury due to bone fragment
migration, callus formation, or hardware irritation.
3. Pathophysiology
- Arterial injury leads to disruption of the intima
and media, while the adventitia or surrounding soft tissues contain the
hemorrhage.
- Blood flow continues into this contained space,
forming a hematoma that maintains communication with the arterial lumen.
- Over time, the hematoma becomes organized and
develops a fibrous wall, lacking the true three-layered arterial wall
(distinguishing it from a true aneurysm).
- Turbulent flow can cause further expansion,
compression of nearby structures, or even rupture.
4. Epidemiology
- Rare complication of femoral fractures; estimated in
<1% of cases.
- More frequent in high-energy trauma or complex
femoral shaft and distal femur fractures.
- Higher incidence in elderly patients (due to
atherosclerosis) and in polytrauma settings.
- Iatrogenic pseudoaneurysms may be increasing due to
higher use of interventional procedures and fixation hardware.
5. Clinical Presentation
Symptoms may appear
immediately or be delayed (days to weeks):
- Painful, expanding mass near the fracture or
surgical site.
- Pulsatile swelling or bruit over the area.
- Neurologic symptoms due to nerve compression
(e.g., numbness, tingling).
- Signs of limb ischemia if distal perfusion is
compromised.
- Hemodynamic instability if the pseudoaneurysm
ruptures.
- Delayed wound healing or recurrent bleeding
post-surgery.
6. Imaging Features
- Doppler Ultrasound: First-line, shows
swirling blood flow ("yin-yang sign"), and neck of
pseudoaneurysm.
- CT Angiography (CTA): Gold standard for
localization, size, and arterial involvement.
- MRI/MRA: Used in some cases, especially to assess soft
tissue involvement.
- Digital Subtraction Angiography (DSA): For diagnostic and
interventional purposes.
7. Treatment
Depends on size, symptoms, and
patient status:
Non-surgical:
- Ultrasound-guided thrombin injection (for small,
well-contained pseudoaneurysms).
- Ultrasound-guided compression (less favored due to
pain and lower success rate).
Endovascular:
- Coil embolization or covered stent
placement – especially in deep or surgically inaccessible
pseudoaneurysms.
Surgical:
- Ligation and repair of the artery (with or
without grafting) during fracture fixation or revision surgery.
- Hematoma evacuation and debridement.
Concurrent fracture
stabilization (if not already performed) is crucial.
8. Prognosis
- Good with early detection and intervention.
- Delayed diagnosis can lead to:
- Rupture and hemorrhagic shock
- Limb ischemia and compartment syndrome
- Infection or osteomyelitis
- Nerve compression injuries
Prognosis worsens in:
- Polytrauma patients
- Delayed or missed pseudoaneurysm diagnosis
- Infected pseudoaneurysms
Long-term follow-up with
imaging may be required, particularly after endovascular repair.
=========================
Case Study: 82-Year-Old Woman with Left Hip Pain After a Fall
Pseudoaneurysm
History and Imaging
-
An 82-year-old woman presented with left hip pain following a fall.
-
She had a history of partial hip arthroplasty due to a right subcapital femoral fracture.
-
She also had a history of intramedullary nailing on the left side for a prior pertrochanteric femoral fracture.
-
Radiographic imaging was performed.
-
X-ray results revealed a displaced periprosthetic fracture of the left femur.
-
She underwent surgery and was discharged a few days later.
Additional Imaging
-
The patient was referred back 10 days later due to fever and a gluteal mass.
-
A soft tissue ultrasound of the buttock was requested.
Quiz 1:
What is the most likely diagnosis?
(1) Particle disease
(2) Abscess
(3) Morel-Lavallée collection
(4) Hematoma and a vascular lesion
Explanation: The presence of a new gluteal mass following recent surgery and trauma, along with systemic signs such as fever, raises concern for a postoperative complication. While infection or soft tissue injury is possible, contrast-enhanced CT demonstrating a vascular lesion suggests a pseudoaneurysm or active bleeding. Hematomas in this region may be complicated by arterial injury, particularly near orthopedic hardware. The timing (delayed presentation after surgery), clinical symptoms (mass and fever), and CT findings (contrast extravasation or focal enhancement in arterial phase) are most consistent with a hematoma associated with a vascular lesion such as a pseudoaneurysm.
CT Imaging
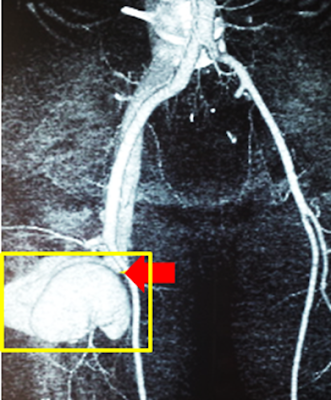
Arterial and venous phase images were obtained sequentially.
Quiz 2:
What does the image demonstrate?
(1) Abscess
(2) Pseudoaneurysm
(3) Active arterial bleeding in the buttock
(4) Active venous bleeding in the buttock
Explanation: The angiographic image shows a well-defined contrast-filled outpouching arising from the inferior gluteal artery, consistent with a pseudoaneurysm. Unlike active bleeding, which typically appears as diffuse extravasation without a defined border, a pseudoaneurysm forms a sac-like structure due to a breach in the arterial wall with blood contained by surrounding tissue. In this case, endovascular coil embolization was the definitive treatment, effectively occluding the lesion and preventing further hemorrhage.
Angiographic Imaging
Arterial angiography was performed, revealing a pseudoaneurysm of the inferior gluteal artery. The lesion was successfully treated with percutaneous coil embolization.
Quiz 3
1. This is a prevalent complication following hip surgery.
(1) True
(2) False
Explanation: Pseudoaneurysm of the gluteal artery is a rare but potentially serious complication following hip surgery or trauma. While other complications, such as infection, dislocation, and thrombosis,s are relatively common, vascular injuries like pseudoaneurysm are uncommon and often underrecognized unless imaging is performed in the presence of unusual symptoms (e.g., swelling, mass, pain, or bleeding).
2. On ultrasound, a characteristic yin-yang sign is seen on color Doppler, and a "to-and-fro" flow pattern is observed on spectral Doppler.
(1) True
(2) False
Explanation: These are hallmark sonographic findings of a pseudoaneurysm. The "yin-yang" sign on color Doppler reflects bidirectional turbulent flow within the pseudoaneurysm sac. The "to-and-fro" pattern on pulse wave Doppler at the neck of the pseudoaneurysm indicates systolic inflow and diastolic outflow, a diagnostic clue of the condition.
3. Inferior gluteal artery pseudoaneurysms are more common than superior gluteal artery pseudoaneurysms.
(1) True
(2) False
Explanation: Superior gluteal artery pseudoaneurysms are more frequently reported in the literature. This is due to the anatomical positioning and proximity of the superior gluteal artery to common surgical fields and injury sites in orthopedic and pelvic procedures. However, both arteries can be involved depending on the mechanism and location of trauma or surgery.
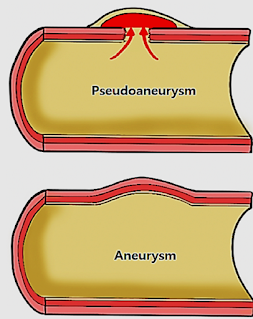
4. A pseudoaneurysm is an abnormal outpouching or expansion of an artery that is confined only by the adventitia or surrounding perivascular soft tissue.
(1) True
(2) False
Explanation: Unlike a true aneurysm, which involves dilation of all three layers of the arterial wall (intima, media, and adventitia), a pseudoaneurysm results from a full-thickness breach in the arterial wall. The adventitia or surrounding tissues contain the blood, forming a pulsatile hematoma with potential communication to the parent artery.
5. On CT imaging, a pseudoaneurysm appears as a hyperdense focal area during the arterial phase and shows progressive washout in later phases.
(1) True
(2) False
Explanation: Contrast-enhanced CT typically reveals a focal hyperattenuating lesion in the arterial phase due to active contrast filling of the pseudoaneurysm sac. As imaging proceeds into the venous and delayed phases, the lesion shows washout, similar to arterial flow dynamics, which helps distinguish it from other soft tissue masses or collections.
Findings and Diagnosis
Findings
Ultrasound imaging revealed a gluteal hematoma accompanied by a vascular lesion demonstrating the characteristic "yin-yang" sign. Spectral Doppler imaging showed a "to-and-fro" waveform, suggestive of a pseudoaneurysm.
On CT imaging, a nodular hyperdense lesion was observed within the gluteal region during the arterial phase, which gradually faded during the venous phase, also indicative of a pseudoaneurysm.
Differential Diagnosis
-
Gluteal hematoma with active arterial bleeding
-
Gluteal hematoma with active venous bleeding
-
Gluteal hematoma with a pseudoaneurysm
Final Diagnosis:
Gluteal hematoma and inferior gluteal artery pseudoaneurysm
Discussion
Pseudoaneurysm (False Aneurysm)
A pseudoaneurysm is an abnormal outpouching or dilation of an artery, characterized by being confined solely to the tunica adventitia or surrounding perivascular soft tissue, rather than involving all three layers of the arterial wall. This distinguishing feature sets it apart from a true aneurysm, which involves the dilation of the intima, media, and adventitia.
Pseudoaneurysms typically develop when there is a disruption in the arterial wall, allowing blood to escape through the intima and media. The extravasated blood is then contained by the outer adventitial layer or surrounding soft tissues, forming a pulsatile hematoma with persistent communication to the artery.
Gluteal artery aneurysms are uncommon, with the superior gluteal artery being the most frequently involved site. In contrast, pseudoaneurysms originating from the inferior gluteal artery are rarely reported in the literature.
Clinical manifestations of gluteal artery pseudoaneurysms are variable and may include localized swelling, pain, and a pulsatile mass. Compression of the sciatic nerve due to mass effect may also occur. The most feared complication is rupture, which can lead to a life-threatening hemorrhage.
Pseudoaneurysms of the gluteal artery can be caused by pelvic fractures, iatrogenic injuries (such as hip arthroplasty, needle biopsy, intramuscular injections, or drainage procedures), or penetrating and blunt trauma (e.g., gunshot or stab wounds).
The interval between trauma and pseudoaneurysm development varies. According to the literature, pseudoaneurysms may become clinically evident within weeks to even years after the initial injury.
The variable time course, mechanism of injury, and nonspecific presentation make pseudoaneurysm a clinically elusive entity. Inappropriate incision and drainage of a pseudoaneurysm mistaken for an abscess or hematoma can result in catastrophic hemorrhage. This case highlights the importance of considering pseudoaneurysm in the differential diagnosis of a firm, fluctuant, warm, and erythematous mass following trauma.
Color Doppler ultrasonography is often the preferred initial imaging modality due to its non-invasive nature and high diagnostic accuracy. Pseudoaneurysms characteristically demonstrate a “yin-yang” sign on color Doppler flow imaging and a “to-and-fro” pattern on spectral Doppler, both of which are key features that help distinguish vascular lesions from other soft tissue abnormalities.
The advent of contrast-enhanced multidetector computed tomography (MDCT) has further enhanced the non-invasive evaluation of traumatic vascular complications, allowing for accurate and rapid diagnosis.
Endovascular treatment via percutaneous selective embolization is widely regarded as the first-line therapy, offering a minimally invasive approach with a low complication rate and significantly reduced risk of iatrogenic sciatic nerve injury. By contrast, open surgical intervention through the gluteus maximus muscle poses a greater risk of hemorrhage and nerve damage.
Some authors propose ultrasound-guided thrombin injection as an alternative, especially in cases involving superficial pseudoaneurysms with narrow necks, such as those seen after femoral arterial catheterization. However, this method carries the inherent risk of thrombin leakage into the arterial circulation, which may lead to severe thrombosis in adjacent vessels.
Key Points
-
Always consider a pseudoaneurysm in the differential diagnosis of post-traumatic soft tissue masses.
-
The onset of a gluteal pseudoaneurysm following trauma can vary widely, from several weeks to several years.
-
Color Doppler ultrasonography may show the yin-yang sign on color flow and a to-and-fro pattern on spectral Doppler.
-
CT angiography typically demonstrates a contrast-filled sac in the arterial phase with gradual washout in the venous phase.
References
- Kobayashi N, Murakami M, Saito T, et al. Pseudoaneurysm of the inferior gluteal artery following blunt trauma: a case report and review of the literature. J Med Case Rep. 2016;10:170. doi:10.1186/s13256-016-0957-6
- Baig W, Rehman A, Ashwood N. Inferior gluteal artery pseudoaneurysm following intramuscular injection: a rare cause of gluteal swelling. BMJ Case Rep. 2012;2012:bcr2012006572. doi:10.1136/bcr-2012-006572
- Branco BC, Boutrous ML, DuBose JJ, et al. Incidence and management of traumatic gluteal artery injuries: a review of the National Trauma Data Bank. Vasc Endovascular Surg. 2013;47(3):198–203. doi:10.1177/1538574413478496
- Alonso-Burgos A, Gonzalez-Herrera L, Martin A, et al. Endovascular treatment of traumatic injuries of the peripheral arteries. Eur J Radiol. 2006;59(3):357–366. doi:10.1016/j.ejrad.2006.04.007
- Saad NEA, Saad WEA, Davies MG, et al. Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics. 2005;25(Suppl 1):S173–S189. doi:10.1148/rg.25si055503







Comments
Post a Comment