Knee Cellulitis
Knee cellulitis is a localized
infection of the skin and subcutaneous tissues around the knee joint. It is an
important clinical entity due to its potential for rapid progression and the
need for prompt recognition and treatment.
1. Cause and Etiology
Cause:
Knee cellulitis is most commonly caused by bacterial infection, typically when
pathogens breach the skin barrier and invade the dermis and subcutaneous
tissues.
Etiology:
- Most common organisms:
- Streptococcus pyogenes (Group A Streptococcus)
– most common
- Staphylococcus aureus, including MRSA
(Methicillin-resistant Staphylococcus aureus)
- Entry points (predisposing
conditions):
- Trauma (abrasions, lacerations, insect bites)
- Post-surgical wound infection (e.g., after knee
arthroscopy or total knee arthroplasty)
- Skin barrier disruption from eczema, psoriasis, and tinea pedis
- Chronic venous insufficiency or lymphedema
- Intravenous drug use
- Diabetes mellitus and immunosuppression
2. Pathophysiology
The pathogenesis of cellulitis
involves the invasion of the dermis and subcutaneous tissues by bacteria,
leading to:
- Inflammatory cascade activation:
- Local release of cytokines (IL-1, TNF-α)
- Neutrophil infiltration
- Tissue edema and erythema due to vasodilation and
increased capillary permeability
- Lymphatic involvement:
- May lead to lymphangitis or lymphedema
- Potential complications:
- Abscess formation
- Bacteremia
- Sepsis
- Septic arthritis occurs if contiguous spread occurs into
the joint
3. Epidemiology
- Incidence: Cellulitis accounts for
approximately 2-3% of hospital admissions annually.
- Age: More common in middle-aged and older adults.
- Gender: Slight male predominance.
- Risk Factors:
- Diabetes mellitus
- Peripheral vascular disease
- Chronic skin conditions (eczema, fungal infections)
- Immunocompromised states
- Previous episodes of cellulitis
- Seasonality: Slightly more common in
warmer months due to increased skin exposure and trauma.
4. Clinical Presentation
Symptoms:
- Localized erythema, swelling, warmth,
and tenderness over the knee
- Fever and malaise (systemic symptoms)
- Pain with movement, particularly in severe cases
Signs:
- Poorly demarcated, erythematous area around the knee
- Possible blistering or purulence
- Regional lymphadenopathy
- May mimic or coexist with deep infections such as:
- Septic arthritis
- Osteomyelitis
- Prepatellar or infrapatellar bursitis
5. Imaging Features
Although cellulitis is
primarily a clinical diagnosis, imaging can help:
a.
Ultrasound:
- First-line modality
- May reveal:
- Thickened subcutaneous tissue
- "Cobblestoning" pattern (due to edema)
- Abscess formation
- Bursitis (e.g., prepatellar)
b. MRI
- High sensitivity for soft tissue and bone
involvement
- T2-weighted images show:
- Subcutaneous hyperintensity (edema)
- Fascial thickening
- Rule out osteomyelitis or septic arthritis
c. CT:
- Useful in emergency settings
- Can show:
- Fluid collections
- Gas-forming infections (e.g., necrotizing
fasciitis)
d.
Radiographs (X-ray):
- Not diagnostic for cellulitis
- Useful for:
- Excluding foreign bodies or fractures
- Assessing bone involvement
6. Treatment
a. Antibiotics (empiric, then
culture-guided):
- Mild to moderate (oral therapy):
- Cephalexin
- Dicloxacillin
- Clindamycin
- TMP-SMX (if MRSA suspected)
- Doxycycline
- Severe cases or systemic signs (IV therapy):
- Cefazolin
- Vancomycin (if MRSA suspected)
- Linezolid or daptomycin in resistant cases
b. Supportive measures:
- Elevation of the affected limb
- Analgesia and anti-inflammatory medications
- Adequate hydration
- Address underlying conditions (e.g., diabetes, tinea
pedis)
c. Surgical intervention:
- Indicated for:
- Abscess drainage
- Debridement (if necrotizing soft tissue infection)
- Septic arthritis if present
7. Prognosis
- Generally favorable with early and
appropriate treatment
- Symptoms typically improve within 48–72 hours of
antibiotic initiation
- Full resolution may take 7–14 days
Poor prognostic factors:
- Delayed treatment
- Recurrent episodes (e.g., chronic lymphedema)
- Immunosuppression or diabetes
- MRSA infection
- Presence of complications (e.g., abscess,
osteomyelitis)
Prevention:
- Proper skin hygiene
- Treatment of fungal infections of the feet
- Compression therapy for chronic lymphedema
- Prophylactic antibiotics for recurrent cases
(controversial)
Reference
1.
Gunderson
CG, Cherry BM, Fisher AK. Clinical and microbiological characteristics of
patients with lower limb cellulitis. Am J Med. 2019 Jan;132(1):e1–e7. doi:10.1016/j.amjmed.2018.06.014
2.
Stevens
DL, Bisno AL. Imaging of soft tissue infection and necrotizing fasciitis: Role
of CT and MRI. Radiographics. 2017 Mar-Apr;37(2):436–450. doi:10.1148/rg.2017160091
3. Liu C, Bayer A,
Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, et al. Clinical practice
guidelines by the Infectious Diseases Society of America for the treatment of
methicillin-resistant Staphylococcus aureus infections in adults and children. Clin
Infect Dis. 2011 Feb;52(1):e18–e55. doi:10.1093/cid/cir367
==================================
Case study: A 56-Year-Old Male with Knee Pain
Knee Cellulitis
History and Imaging Findings
-
A 56-year-old male presented with persistent pain in his left knee.
-
The patient had a significant history of multiple episodes of effusion in the left knee.
-
Previous joint aspiration tests revealed no evidence of infection.
-
There was no history of trauma to the knee. He visited the clinic seeking evaluation and management of the pain.
-
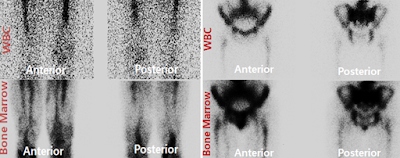
Nuclear medicine imaging was performed for further evaluation, including tagged white blood cell (WBC) and bone marrow scintigraphy.
Quiz
Which of the following represents the most significant finding?
(1) Left femoral osteomyelitis
(2) Left knee osteomyelitis
(3) Left knee soft tissue infection (cellulitis)
(4) Physiological tracer uptake is not indicative of infection
Explanation:
The nuclear medicine imaging showed increased radiotracer activity in the soft tissues around the left knee without focal bony involvement, which is most consistent with cellulitis rather than osteomyelitis.
Which radiotracer is used in tagged white blood cell (WBC) imaging?
(1) Technetium-99m (99mTc)
(2) Fluorine-18 fluorodeoxyglucose (18F-FDG)
(3) Indium-111 (111In)
(4) Iodine-123 (123I)
Explanation:
Indium-111-labeled leukocytes are commonly used for WBC scintigraphy, particularly in detecting and localizing infections such as osteomyelitis or soft tissue abscesses.
Which radiotracer is typically used for bone marrow imaging?
(1) Technetium-99m (99mTc)
(2) Fluorine-18 fluorodeoxyglucose (18F-FDG)
(3) Indium-111 (111In)
(4) Iodine-123 (123I)
Explanation:
Technetium-99m sulfur colloid is the preferred agent for bone marrow scintigraphy due to its ability to localize in the reticuloendothelial system, providing a reference for differentiating between normal marrow uptake and infection.
What is the half-life of the radiotracer used in tagged WBC imaging?
(1) 109.7 minutes
(2) 6 hours
(3) 13.2 hours
(4) 2.8 days
Explanation:
Indium-111 has a physical half-life of approximately 2.8 days, allowing for delayed imaging at 24–48 hours post-injection to optimize infection detection.
Which of the following indicates a positive result for osteomyelitis?
(1) Spatially congruent activity on both WBC and marrow images at the same osseous site
(2) Spatially discordant activity between WBC and marrow images at the same osseous site
Explanation:
A discordant pattern (increased uptake on WBC scan without corresponding uptake on marrow scan) is highly suggestive of osteomyelitis, as normal marrow activity would be preserved if the area were non-infected.
In a separate marrow study, there is notable urinary bladder activity on pelvic imaging, and matching activity is seen in a large joint on both WBC and marrow scans. What does this suggest to the clinician?
(1) The findings may be interpreted as negative for osteomyelitis
(2) The findings cannot be definitively interpreted as negative for osteomyelitis
Explanation:
When WBC and marrow scans show matching activity, this suggests that the uptake is physiologic or related to normal marrow, not infection. Therefore, the study can be interpreted as negative for osteomyelitis in that location.
Findings and Diagnosis
Findings:
Indium-111-labeled white blood cell (¹¹¹In WBC) and Technetium-99m sulfur colloid bone marrow scans demonstrated mild and diffuse uptake in the soft tissues of the left knee. There was no corresponding uptake in the adjacent bone structures, indicating discordance. These findings are suggestive of a soft tissue infection such as cellulitis, rather than osteomyelitis.
Differential Diagnosis
In evaluating a patient presenting with left knee pain and swelling, the following differential diagnoses should be considered:
-
Left Knee Cellulitis: An acute bacterial infection of the skin and subcutaneous tissues, often presenting with localized erythema, warmth, swelling, and tenderness.
-
Left Knee Osteomyelitis: A bone infection that may present with similar symptoms but typically involves deeper structures, including bone marrow.
-
Left Knee Fracture: A structural injury to the bone that can present with pain and swelling, often following trauma.
Diagnosis: Left Knee Cellulitis
Based on clinical presentation and imaging findings, the diagnosis is consistent with left knee cellulitis.
Discussion
Pathophysiology
Cellulitis is a common bacterial skin infection involving the deep dermis and subcutaneous tissue. It typically results from the entry of bacteria through breaches in the skin barrier, leading to an inflammatory response characterized by erythema, warmth, swelling, and pain. The most common causative organisms are Streptococcus pyogenes and Staphylococcus aureus.
In adults, hematopoiesis primarily occurs in the bone marrow, leading to significant uptake of radiolabeled white blood cells (WBCs) in these areas during nuclear imaging. However, in the presence of infection, WBCs accumulate at the site of infection, which can be detected using radiolabeled WBC scans. It's important to note that WBCs do not typically accumulate in areas of increased bone turnover unless infection is present.
Clinical Presentation
Patients with cellulitis often present with:
-
Pain: Localized to the affected area.
-
Swelling: Due to inflammation and edema.
-
Redness (Erythema): Resulting from increased blood flow.
-
Warmth: Due to inflammation.
-
Weakness: In the affected limb.
-
Pus: In cases where an abscess has formed.
Imaging Features
Nuclear Medicine Imaging:
-
Indium-111-labeled WBC Scan: Shows increased uptake in areas of infection due to accumulation of labeled leukocytes.
-
Technetium-99m Sulfur Colloid Bone Marrow Scan: Demonstrates normal bone marrow distribution.
In cellulitis, both scans show concordant uptake in the soft tissues without bone involvement, indicating soft tissue infection. In contrast, osteomyelitis typically presents with discordant findings: increased uptake on the WBC scan and reduced or absent uptake on the sulfur colloid scan in the affected bone, suggesting bone marrow involvement.
MRI:
-
Cellulitis: Demonstrates diffuse soft tissue edema and enhancement without bone marrow involvement.
-
Osteomyelitis: Shows bone marrow edema, cortical destruction, and possible abscess formation.
Treatment
-
Antibiotic Therapy: Empirical broad-spectrum antibiotics targeting common pathogens, adjusted based on culture results.
-
Surgical Intervention: Incision and drainage in cases where an abscess is present.
-
Supportive Care: Elevation of the affected limb, pain management, and monitoring for systemic involvement.
References
-
Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(2):e10-e52. doi:10.1093/cid/ciu296.
-
Elgazzar AH, et al. Indium-111-labeled leukocyte and technetium-99m sulfur colloid imaging in the evaluation of suspected osteomyelitis. J Nucl Med. 1996;37(5):858-864.
-
Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004;364(9431):369-379. doi:10.1016/S0140-6736(04)16727-5.
-
Pineda C, Espinosa R, Pena A. Radiographic imaging in osteomyelitis: the role of plain radiography, computed tomography, ultrasonography, magnetic resonance imaging, and scintigraphy. Semin Plast Surg. 2009;23(2):80-89. doi:10.1055/s-0029-1214160.
-
Tice AD, et al. Comparative effectiveness of antibiotic treatment strategies for osteomyelitis: a retrospective cohort study. BMC Infect Dis. 2011;11:75. doi:10.1186/1471-2334-11-75.





Comments
Post a Comment