Acute Abdominal Aortic Occlusion (AAAO) due to Embolism from a Left Atrial Myxoma
1. Cause and Etiology
Left atrial myxoma is the most common primary
cardiac tumor, typically benign and arising from the interatrial septum near
the fossa ovalis. While they can cause symptoms via intracardiac obstruction or
constitutional effects, a significant complication is embolization.
- Etiology of AAAO in this context:
- Embolic obstruction of the abdominal aorta
due to a tumor fragment or thrombus originating from the surface of a
left atrial myxoma.
- Emboli from myxomas are friable and gelatinous, and they are more likely to lodge in large or medium-sized arteries like the abdominal aorta or its major branches.
2. Pathophysiology
- Tumor embolization occurs when fragments of
the myxoma or superimposed thrombi dislodge and enter the systemic
circulation.
- In AAAO:
- The embolus travels down the aorta and lodges at or
below the aortic bifurcation (e.g., aortoiliac segment),
causing complete or near-complete occlusion.
- Ischemia of the lower limbs and pelvic organs
occurs, leading to a rapid onset of symptoms.
- Collateral circulation is often insufficient
to prevent ischemia due to the sudden nature of the blockage.
3. Epidemiology
- Left atrial myxoma incidence: ~0.5 per
million population annually.
- Systemic embolization occurs in 30–40% of
myxoma patients; cerebral and peripheral embolism is common.
- Acute aortic occlusion is rare (<1% of all
arterial embolisms) and most often caused by thromboembolism, with cardiac
sources like atrial fibrillation more common than myxomas.
- AAAO due to myxoma embolism is extremely rare, with
only isolated case reports in the literature.
4. Clinical Presentation
Patients typically present
with features of acute aortic syndrome and lower limb ischemia:
- Sudden onset of bilateral lower limb pain and weakness
- Paralysis or paraparesis
- Pallor, cold limbs, mottled skin
- Absent femoral/popliteal pulses
- Lower abdominal or flank pain
- Anuria or oliguria (renal hypoperfusion)
- Possible constitutional symptoms (if myxoma has
systemic effects):
- Fever, weight loss, malaise
- Signs of emboli elsewhere (e.g., stroke, splenic
infarct)
5. Imaging Features
A. Cardiac Imaging (to detect
the myxoma):
- Transthoracic or Transesophageal Echocardiography:
- Mobile, echogenic mass attached to the interatrial
septum (left atrial side)
- Pedunculated, often prolapses into the mitral valve
orifice
B. Vascular Imaging:
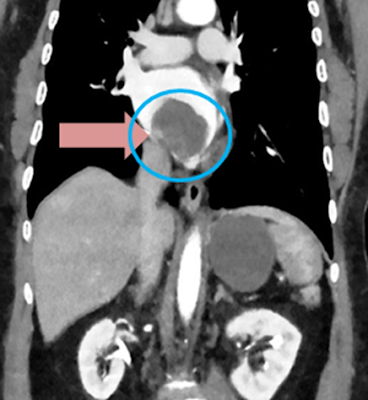
- CT Angiography (CTA):
- Abrupt occlusion of the abdominal aorta at or near
the bifurcation
- Lack of contrast enhancement distal to the
occlusion
- May show "saddle embolus" at the
aortoiliac junction
- Absence of atherosclerosis may suggest embolic
etiology
- MRI or MRA (less common in acute
setting)
- Duplex ultrasound: May help identify
absent flow in distal vessels
6. Treatment
Emergency intervention is
essential to prevent permanent ischemia and death.
A. Initial stabilization:
- Intravenous fluids
- Anticoagulation with heparin (if no
contraindications)
B. Definitive treatment:
- Surgical embolectomy:
- Transabdominal or transfemoral approach
- Removal of embolus via Fogarty balloon catheter
- Restoration of perfusion to lower limbs and organs
- Aortic bypass or endovascular therapy (if surgical embolectomy
fails or is incomplete)
- Cardiac surgery (after stabilization):
- Excision of the left atrial myxoma via median sternotomy
- Prevents recurrence of embolization
C. Supportive care:
- Management of acute kidney injury, metabolic
acidosis
- Intensive care monitoring
7. Prognosis
- Highly time-sensitive: The mortality rate for AAAO
can reach 75% if not promptly treated.
- Better outcomes with:
- Early diagnosis
- Rapid surgical embolectomy
- Removal of cardiac myxoma
- Delayed treatment can lead to:
- Limb loss
- Multi-organ failure
- Irreversible paraplegia
Recurrence risk:
- After complete surgical excision of myxoma: <5%
- Regular follow-up with echocardiography is required
to monitor for recurrence
References (suggested for
deeper reading):
- Reynen K. Cardiac myxomas. N Engl J Med.
1995;333(24):1610-7.
- Di Eusanio M et al. Surgical treatment of primary
cardiac tumors: 25 years of experience. Ann Thorac Surg. 2000.
- Criado E et al. Acute aortic occlusion: a 40-year
experience. J Vasc Surg. 2002;35(5):958–63.
- Patel J et al. Left atrial myxoma presenting with
embolic occlusion of the abdominal aorta. Vascular. 2006.
- Livi U et al. Massive embolism of the abdominal
aorta caused by an atrial myxoma. J Cardiovasc Surg. 1988.



Comments
Post a Comment