Acquired Pulmonary Vein Stenosis
Case Overview
A 60-year-old woman presented with intermittent left-sided chest pain and hemoptysis that had persisted for several weeks. Her medical history included paroxysmal atrial fibrillation, for which she underwent catheter ablation four months prior. A chest radiograph revealed minimal left-sided pleural effusion with stable parenchymal scarring but no focal consolidation.
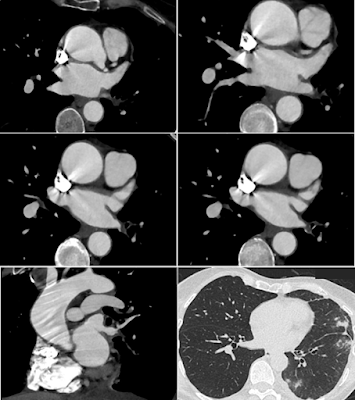
Subsequent CT angiography (CTA) revealed severe focal stenosis in the superior segment of the left inferior pulmonary vein, and possible occlusion or high-grade stenosis in the basal segment. Multifocal ground-glass opacities (GGO) and peripheral consolidation were noted in the left lower lobe and lingula, raising suspicion for pulmonary venous congestion.
Differential Diagnosis
-
Pulmonary vein stenosis (PVS)
-
Pulmonary vein thrombosis
-
Pulmonary vein atresia
-
Tumor thrombus involving the pulmonary vein
The final diagnosis was acquired pulmonary vein stenosis, most likely secondary to prior radiofrequency ablation.
Discussion
1. Pathophysiology
Acquired pulmonary vein stenosis (PVS) is most commonly a consequence of iatrogenic injury, particularly radiofrequency catheter ablation for atrial fibrillation. The mechanism involves thermal damage to the venous endothelium, followed by fibrosis, resulting in progressive luminal narrowing. Other causes include:
-
Malignant infiltration (primary lung cancer, lymphoma, metastases)
-
Benign external compression (fibrosing mediastinitis, sarcoidosis, mediastinal cysts)
-
Post-surgical or congenital causes
Luminal narrowing leads to pulmonary venous hypertension, resulting in alveolar hemorrhage, interstitial edema, and eventually parenchymal fibrosis if untreated.
2. Epidemiology
-
Acquired PVS is rare, with an increased incidence following the rise in catheter-based ablation procedures.
-
Studies suggest 3%–5% of patients may develop significant PVS after ablation, with many being asymptomatic unless >70% of the lumen is narrowed.
-
Bilateral or multivessel involvement has been reported in 10–20% of post-ablation cases.
3. Clinical Presentation
Symptoms may be non-specific and often mimic pulmonary embolism or infection, delaying diagnosis:
-
Dyspnea on exertion
-
Non-productive cough
-
Pleuritic chest pain
-
Hemoptysis (seen in ~20–30% of cases)
-
Rarely: recurrent pneumonia or pulmonary hypertension
Symptom onset typically occurs weeks to months post-ablation.
4. Imaging Features
CT Angiography (CTA) is the modality of choice for diagnosis. Key findings include:
-
Focal narrowing or occlusion of pulmonary veins
-
Delayed contrast opacification of the affected vein
-
Ground-glass opacities and septal thickening in the corresponding lung segment
-
Pleural effusion, particularly ipsilateral to the stenosed vein
MRI can offer functional information (flow dynamics) but is less widely available and slower than CT.
Chest X-ray may show indirect signs such as unilateral pleural effusion or subtle interstitial opacities.
5. Treatment
Treatment decisions depend on symptom severity and degree of stenosis:
| Severity | Treatment Options |
|---|---|
| Asymptomatic or mild | Observation with serial imaging |
| Symptomatic / >70% stenosis | Balloon angioplasty, stenting |
| Refractory or complex cases | Surgical venoplasty or lobectomy |
6. Prognosis
-
Early detection and intervention can prevent chronic pulmonary hypertension and parenchymal damage.
-
Prognosis is generally good if treated before irreversible changes.
-
Restenosis rates vary depending on the technique and stent type.
Conclusion
Acquired pulmonary vein stenosis is a rare but potentially serious complication following catheter ablation for atrial fibrillation. Awareness of its clinical and radiologic manifestations—particularly unilateral ground-glass opacities and venous narrowing on CTA—is vital for timely diagnosis and management. Endovascular therapy remains the cornerstone of treatment, with excellent outcomes when implemented early.
Quiz
1. What radiologic finding was present on chest X-ray?
A. Hampton’s hump
B. Parenchymal scarring
C. Focal consolidation
D. Overt pulmonary edema
Explanation: The chest X-ray showed stable parenchymal scarring on the left without focal consolidation or signs of edema.
2. What was the main abnormality noted on CTA?
A. Left atrial aneurysm
B. Subsegmental pulmonary embolism
C. Left atrial appendage thrombus
D. Pulmonary vein stenosis
Explanation: CTA revealed severe stenosis in the left inferior pulmonary vein, consistent with post-ablation PVS.
3. What likely causes the ground-glass opacities and pleural effusion?
A. Vasculitis
B. Metastatic disease
C. Venous congestion
D. Septic embolism
Explanation: PVS leads to localized pulmonary venous congestion, resulting in ground-glass attenuation and pleural effusion.
4. Is open surgical correction the preferred treatment for symptomatic PVS?
A. True
B. False
Explanation: Minimally invasive techniques such as balloon angioplasty and stenting are currently the preferred initial treatments.
References
-
Saad EB, Marrouche NF, Saad CP, et al. Pulmonary vein stenosis after catheter ablation of atrial fibrillation. Circulation. 2003;108(25):3102-3107. doi:10.1161/01.CIR.0000103126.62084.96
-
Prieto LR, Schoenhagen P, Arruda MJ, et al. Pulmonary vein stenosis complicating ablation of atrial fibrillation: functional characterization, evolution, and response to angioplasty. J Cardiovasc Electrophysiol. 2003;14(4):439-445.
-
Di Biase L, Natale A. Pulmonary vein stenosis after ablation of atrial fibrillation: clinical implications and treatment. J Am Coll Cardiol. 2010;56(9):712-722. doi:10.1016/j.jacc.2010.03.065
-
Linhart M, Gutfried P, Horlbeck FW, et al. Acquired pulmonary vein stenosis: etiology, diagnosis, and treatment options. J Thorac Dis. 2018;10(1):E49-E56. doi:10.21037/jtd.2017.12.63
-
Mehra D, Zoghbi WA, Little SH. Pulmonary vein stenosis: pathophysiology, diagnosis, and intervention. Eur Heart J Cardiovasc Imaging. 2017;18(4):450-457. doi:10.1093/ehjci/jew202


Comments
Post a Comment