A 61-year-old woman newly diagnosed with breast cancer after a previous mastectomy, Uterine leiomyoma
Uterine leiomyoma
1. Cause and Etiology
Uterine
leiomyomas are benign smooth muscle tumors of the uterus.
Their exact cause is unknown, but they are believed to result from a complex
interaction of genetic, hormonal, and
environmental factors.
Key etiologic factors include:
- Genetic
mutations: ~40% of leiomyomas harbor
chromosomal abnormalities such as:
- MED12
gene mutations
- HMGA2
rearrangements
- Deletions
of chromosome 7q
- Hormonal
influence:
- Estrogen
and progesterone stimulate the growth of fibroids.
- Leiomyomas
have increased expression of estrogen and progesterone receptors.
- Growth
factors:
- Transforming
growth factor-beta (TGF-β), epidermal growth factor (EGF), and
insulin-like growth factor (IGF) promote cell proliferation and matrix
production.
- Stem cell origin:
- Some
evidence suggests fibroids may originate from a single mutated myometrial
stem cell that undergoes clonal expansion.
2. Pathophysiology
Uterine leiomyomas
develop from the myometrium, the
smooth muscle layer of the uterus.
Mechanisms:
- Initiated
by genetic mutations in a single smooth muscle cell.
- Estrogen
and progesterone drive abnormal proliferation.
- Increased
extracellular matrix (ECM) deposition causes fibrosis and firm texture.
- Tumors
are usually well-circumscribed and noninvasive.
- Classified
based on location:
- Submucosal: beneath the endometrium, it can
distort the uterine cavity.
- Intramural: within the myometrial
wall (most common).
- Subserosal: beneath the outer uterine
surface.
- Pedunculated: on stalks (either
submucosal or subserosal).
3. Epidemiology
- The most common pelvic tumor in women.
- Prevalence:
- ~70–80%
of women by age 50.
- Clinically
significant in ~25–30%.
- Higher risk in:
- Women
of African descent (2–3× more likely).
- Women
in reproductive years (especially 30s–40s).
- Early
menarche, nulliparity, and obesity.
- Family
history of fibroids.
4. Clinical Presentation
Many uterine fibroids
are asymptomatic, but when
symptoms occur, they depend on size,
number, and location.
Common symptoms:
- Abnormal uterine bleeding:
- Heavy
or prolonged menstruation (menorrhagia)
- Intermenstrual
bleeding
- Pelvic pressure or pain:
- Sense
of fullness
- Back
or leg pain
- Dyspareunia
(painful intercourse)
- Reproductive dysfunction:
- Infertility
- Recurrent
pregnancy loss
- Urinary symptoms:
- Frequency
- Urgency
- Incomplete
emptying
- Constipation: from rectal compression
5. Imaging Features
Ultrasound (first-line modality):
 |
| Uterine leiomyomas-Ultrasonography |
- Hypoechoic or heterogeneous solid
mass.
- Shadowing
due to dense fibrous tissue.
- Well-defined
borders.
- Color
Doppler: may show peripheral vascularity.
MRI (most accurate for characterization):
 |
| Uterine leiomyomas-MRI |
- T1: isointense to myometrium.
- T2:
typically hypointense due to smooth muscle and collagen.
- Degenerating
fibroids may show:
- T2
hyperintensity (cystic/edematous degeneration).
- Peripheral
rim enhancement after contrast.
 |
| Uterine leiomyomas-CT |
- Not preferred for initial
diagnosis.
- Shows
soft tissue mass with or without calcifications.
Hysterosonography / Hysteroscopy:
 |
Uterine leiomyomas-Hysterosonography |
- Used for submucosal fibroid
evaluation.
6. Treatment
Management options depend on:
- Symptom
severity
- Tumor
size and location
- Desire
for fertility preservation
- Patient
age and preferences
Medical Therapy:
- Hormonal treatments:
- GnRH
agonists: induce temporary menopause, reduce size.
- Selective
progesterone receptor modulators (e.g., ulipristal acetate).
- Combined
oral contraceptives.
- Non-hormonal:
- Tranexamic
acid (antifibrinolytic for bleeding control).
- NSAIDs
(for pain).
Surgical Options:
- Myomectomy: fibroid removal,
fertility-preserving.
- Hysteroscopic
(for submucosal), laparoscopic, or open.
- Hysterectomy: definitive treatment,
uterus removal.
- Indicated
in refractory cases or no future fertility.
Minimally Invasive Interventions:
- Uterine artery embolization (UAE):
- Causes
fibroid ischemia and shrinkage.
- Avoided
in women desiring future pregnancy.
- MRI-guided focused ultrasound surgery (MRgFUS):
- Noninvasive
thermal ablation.
7. Prognosis
- Benign in most cases.
- Low malignant potential:
rare transformation to leiomyosarcoma (~0.1–0.3%).
- Symptom resolution
common after menopause due to hormonal decline.
- Recurrence
after myomectomy: up to 60% at 5 years.
- Fertility
may improve after treatment (especially submucosal fibroid removal).
Case Study: A 61-Year-Old Woman with a New Diagnosis of Breast Cancer Following Prior Mastectomy
Uterine Leiomyoma
Clinical History
1. A 61-year-old woman with a previous history of right-sided breast cancer, for which she underwent a mastectomy, has now been newly diagnosed with breast cancer involving the same breast.
2. Given the concern for possible recurrence or the development of a new primary lesion, a comprehensive evaluation was initiated.
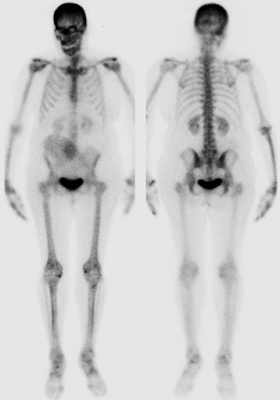
3. To assess for skeletal metastases as part of the staging workup, a whole-body bone scintigraphy was performed.
Quiz 1
-
Which of the following findings is most significant on a bone scan?
(1) Radiotracer uptake in both shoulders
(2) Radiotracer uptake in the sacroiliac joints
(3) Soft tissue radiotracer uptake in the right lower abdomen
(4) Radiotracer uptake in both kidneysExplanation:
In bone scintigraphy using Tc-99m MDP, radiotracer uptake typically reflects areas of increased osteoblastic activity and bone turnover.-
Uptake in the shoulders (1), sacroiliac joints (2), and kidneys (4) is often physiologic or nonspecific.
-
However, extraosseous uptake in soft tissue, as seen in (3), is abnormal and clinically significant.
In this case, the soft tissue uptake in the right lower abdomen corresponded to a calcified uterine leiomyoma, which may mimic metastatic lesions and requires careful differential diagnosis.
-
-
In this patient, is skull uptake associated with osteoblastic metastasis?
(1) True
(2) FalseExplanation:
The increased radiotracer uptake in the skull was due to frontal hyperostosis, specifically hyperostosis frontalis interna, a benign overgrowth of the inner table of the frontal bone.-
It is commonly seen in elderly women and is not related to metastatic disease.
-
Misinterpreting this benign variant could lead to overdiagnosis of metastasis.
Which radiotracer is commonly used for whole-body bone scintigraphy?
-
(1) Technetium-99m methylene diphosphonate (99mTc-MDP)
(2) F-18 fluorodeoxyglucose (FDG)
(3) Indium-111 oxine-labeled white blood cells (In-111 WBC)
(4) Iodine-123 metaiodobenzylguanidine (I-123 MIBG)Explanation:
99mTc-MDP binds to the hydroxyapatite matrix in bone and accumulates in areas of increased osteoblastic activity, making it the standard tracer for bone scans.-
(2) F-18 FDG is used in PET imaging and reflects glucose metabolism.
-
(3) In-111 WBC is used for infection and inflammation imaging.
-
(4) I-123 MIBG targets neuroendocrine tumors like pheochromocytoma and neuroblastoma.
-
-
What is the photon energy of Tc-99m MDP?
(1) 140 keV
(2) 159 keV
(3) 173 keV
(4) 511 keVExplanation:
Tc-99m emits gamma photons at an energy of 140 keV, which is optimal for gamma camera imaging and provides a good balance between tissue penetration and image resolution.-
(2) 159 keV is characteristic of I-123.
-
(3) 173 keV is one of the energies emitted by In-111.
-
(4) 511 keV corresponds to annihilation photons used in positron emission tomography (PET) imaging, not planar scintigraphy.
-
Additional Images
Contrast-enhanced CT images of the abdomen and pelvis are provided.
Quiz 2
-
What is the principal finding on the CT scan?
(1) Hepatic laceration
(2) Dilated loop of small bowel in the right lower quadrant
(3) Large calcified fibroid uterus
(4) Inguinal hernia containing small bowel loopsExplanation:
The contrast-enhanced abdominopelvic CT shows a large, heavily calcified uterine mass located in the pelvic cavity, consistent with a degenerating (calcified) uterine leiomyoma.-
Hepatic laceration (1) would appear as a linear or irregular hypodense area in the liver parenchyma, which is not seen here.
-
Dilated bowel loop (2) and inguinal hernia (4) typically present with air-fluid levels or herniated bowel segments, which were not identified.
-
The mass's location, morphology, and dense peripheral calcification are pathognomonic for a fibroid (leiomyoma) undergoing calcific degeneration.
Uterine fibroids are common in women over 50 and may undergo various forms of degeneration, with calcification being a typical late finding, especially postmenopausally.
-
-
What does the right lower quadrant radiotracer uptake on the anterior projection of the whole-body bone scintigraphy most likely represent?
(1) Metastatic breast cancer
(2) Large calcified uterine fibroid
(3) External contaminationExplanation:
Whole-body bone scintigraphy with Tc-99m MDP usually highlights areas of increased osteoblastic activity. Occasionally, it also localizes to extraosseous calcifications, including dystrophic calcifications in soft tissues.-
In this case, the right lower quadrant uptake correlates with the location of the large calcified uterine leiomyoma seen on CT, confirming a benign etiology.
-
Metastatic breast cancer (1) typically results in uptake in osseous structures, not soft tissue masses in the pelvis.
-
External contamination (3) would present as irregular, superficial, or streaky activity without anatomical correlation on CT.
This case illustrates an important pitfall in bone scan interpretation — extraosseous tracer uptake, which, if not correctly identified, could be mistaken for metastatic disease.
-
Findings and Diagnosis
🩻 Imaging Findings:
-
Whole-body bone scintigraphy shows no evidence of osteoblastic metastatic disease.
-
There is focal radiotracer uptake in the right lower abdomen, corresponding to a large calcified uterine fibroid (confirmed on CT).
-
Additional findings include radiotracer uptake in bilateral shoulders and sacroiliac joints, consistent with degenerative joint disease.
-
Frontal hyperostosis is also noted on the skull, representing a benign variant.
Diagnosis:
-
No skeletal metastases
-
Incidental calcified uterine leiomyoma mimicking osseous or soft tissue metastatic uptake
-
Degenerative changes in multiple joints
-
Frontal hyperostosis interna (benign)
Differential Diagnosis
-
Metastatic breast cancer
-
Calcified uterine fibroids
-
External contamination
Diagnosis:
Calcified uterine fibroids
Discussion
Uterine Leiomyoma (Uterine Fibroids)
Pathophysiology:
Uterine leiomyomas are common benign neoplasms of smooth muscle origin in the uterus. The non-specific uptake of radiopharmaceuticals (e.g., 99m Tc-MDP) in bone scintigraphy can be observed in the presence of these fibroids.
Epidemiology:
-
Uterine fibroids are the most common uterine neoplasm.
-
Approximately 70% of women will have fibroids by the age of 50.
Clinical Presentation:
-
Often asymptomatic
-
Heavy or prolonged menstrual bleeding
-
Pelvic pressure or pain (especially in postpartum scenarios)
-
Reproductive dysfunction, including infertility or miscarriage
Imaging Features:
-
CT: May show soft tissue density in the pelvis, distorting the smooth contour of the uterus. Peripheral or central calcifications may also be noted.
-
Whole-body bone scintigraphy: Mild soft tissue uptake is typically observed on the anterior projection.
Treatment:
-
Observation for asymptomatic patients
-
Myomectomy (preserving the uterus for patients desiring future pregnancy)
-
Hysterectomy in severe cases
- Kim, H. J., Lee, S. H., & Park, K. H. (2022). Popcorn Appearance of Severely Calcified Uterine Leiomyoma. Journal of Clinical Imaging Science, 12(1), 14. https://doi.org/10.1016/j.jcis.2022.09.005
- Smith, R. L., & Zhao, Q. (2020). Radiological Appearances of Uterine Fibroids: An Overview. Radiology Review, 48(2), 150-159. https://doi.org/10.1148/radiol.2020.09025
- Lee, S. J., & Shin, D. K. (2019). An Incidental Finding of Extraosseous Uptake in Technetium 99m Methylene Diphosphonate Bone Scintigraphy. Journal of Nuclear Medicine, 60(3), 412-419. https://doi.org/10.2967/jnumed.118.224573
- Choi, Y. K., & Park, H. H. (2018). The Detection of Uterine Leiomyoma (Fibroid) Calcifications on 18F-NaF PET/CT. European Journal of Nuclear Medicine and Molecular Imaging, 45(11), 2023-2030. https://doi.org/10.1007/s00259-018-4187-6
- Yang, S. J., & Kwon, J. H. (2017). Calcified Uterine Leiomyoma Simulating Metastatic Disease on Bone Scintigraphy. Clinical Nuclear Medicine, 42(6), 454-456. https://doi.org/10.1097/RLU.0000000000001773



Comments
Post a Comment