Lipohemarthrosis of the Knee
1. Definition
Lipohemarthrosis
refers to the presence of both fat and blood within a joint space,
most commonly seen in the knee joint, typically following intra-articular
fractures. The fat originates from bone marrow, while the blood
results from vascular injury associated with the fracture.
2. Cause and Etiology
Primary cause:
- Intra-articular fracture
of a bone containing marrow fat, usually:
- Distal femur
- Proximal tibia
- Patella
Mechanism:
- A fracture extends into the joint
space.
- Marrow elements (including fat) and
blood leak into the synovial cavity.
- The fat separates from the blood
due to differences in density and buoyancy.
Common etiologic
events:
- Trauma (e.g., falls, motor vehicle
accidents, sports injuries)
- Rarely, non-traumatic causes such
as:
- Pathological fractures
(e.g., due to bone tumors or osteomyelitis)
3. Pathophysiology
- Fracture of an intra-articular bone
disrupts both the bone marrow and the intraosseous blood vessels.
- Fat droplets from marrow and hemorrhage
enter the joint space.
- Due to specific gravity,
the components stratify:
- Fat (least dense)
floats to the top
- Serum (middle layer)
- Red blood cells (most dense)
settle at the bottom
- This leads to the characteristic fat-fluid
level, which may be visible on imaging.
Important
pathophysiologic note:
- A visible fat-fluid level confirms
the fracture is intra-articular, even when the fracture line is
not apparent on plain radiographs.
4. Epidemiology
- Most common joint affected:
Knee
- Demographics:
- More common in young
adults and adolescents due to higher rates of high-energy
trauma.
- Occurs in both sexes,
slightly more in males due to trauma patterns.
- Incidence: Not precisely known, but
lipohemarthrosis is observed in up to 40% of knee
effusions associated with intra-articular fractures.
5. Clinical Presentation
Symptoms:
- Acute knee pain
- Swelling and effusion
- Limited range of motion
- Hemarthrosis (blood in the joint)
- Occasionally, joint
instability
Signs:
- The joint appears tense and swollen
- May have positive
ballottement sign
- May show ecchymosis
over the patella or joint line
History often
reveals:
- Recent trauma, such as a direct
blow to the knee or a fall
6. Imaging Features
Plain Radiography (X-ray)
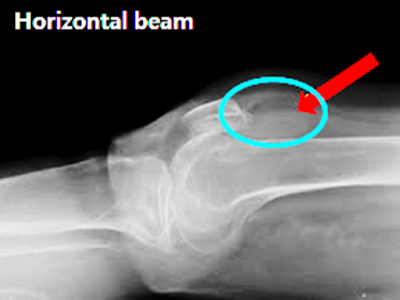
- Cross-table lateral view
of the knee is most sensitive
- Detects fat-fluid level
in the suprapatellar pouch
- Requires a horizontal beam
with the patient in the supine position
- A visible level suggests an intra-articular fracture, even if the fracture line is subtle
Computed Tomography (CT)
- More sensitive for detecting:
- Subtle or occult intra-articular
fractures
- Fat-fluid levels with better
definition than X-ray
- Often used for preoperative
planning
Magnetic Resonance
Imaging (MRI)
- Not typically first-line, but can:
- Confirm lipohemarthrosis
- Visualize associated ligament,
meniscal, or cartilage injuries
Ultrasound (US)
- May detect joint effusion but is not
specific for fat-fluid levels
7. Treatment
Primary goals:
- Address the underlying fracture
- Manage joint effusion
(drainage rarely needed unless symptomatic)
- Prevent complications (e.g.,
infection, stiffness)
Management depends on
fracture type:
- Non-displaced fractures:
Conservative treatment (immobilization, rest, NSAIDs)
- Displaced intra-articular fractures:
May require surgical fixation
Supportive care:
- Ice, elevation, analgesics
- Restricted weight-bearing
- Physical therapy is used after healing to
regain motion and strength
Joint aspiration:
- Typically not required
unless:
- Suspicion of infection (e.g.,
septic arthritis)
- Severe pain due to distension
8. Prognosis
Short-term outlook:
- Generally good with prompt
treatment
- Lipohemarthrosis itself does
not cause permanent damage, but the associated fracture
may influence the outcome
Long-term prognosis
depends on:
- Severity and location of the fracture
- Adequacy of reduction (if
surgically treated)
- Presence of soft tissue or
cartilage injury
- Early mobilization and
rehabilitation
Potential complications:
- Post-traumatic osteoarthritis
- Joint stiffness
- Chronic pain or effusion
- Rarely, fat embolism
syndrome (systemic risk with long bone fractures)
Summary Table
|
Aspect |
Details |
|
Cause |
Intra-articular
fracture (distal femur, proximal tibia, patella) |
|
Pathophysiology |
Marrow fat and blood
enter joint → stratify into fat-fluid level |
|
Epidemiology |
Common in trauma
patients, especially young males |
|
Presentation |
Pain, swelling,
effusion, limited motion |
|
X-ray |
Fat-fluid level on
cross-table lateral knee radiograph |
|
CT |
Sensitive for subtle
fractures and fluid levels |
|
MRI |
Helpful for
associated soft tissue injuries |
|
Treatment |
Treat underlying
fracture; conservative or surgical as indicated |
|
Prognosis |
Generally good;
depends on fracture severity and management |
===================================================
Case Study: A 57-Year-Old Woman with Knee Pain
-
A 57-year-old woman with a history of myopathy presented with right knee pain after a fall.
-
She was unable to bear weight on her right leg following the fall.
-
She reported no numbness or tingling in the right lower extremity.
-
Physical examination of the right knee revealed abrasions, tenderness to palpation of the patella, swelling, and inability to perform a straight leg raise due to pain.
-
Anteroposterior and lateral radiographs of the right knee were obtained.
Quiz 1
1. Which of the following is the most appropriate indication for initial imaging of this patient's injured knee?
(1) Fall
(2) Twisting of the knee
(3) Skin abrasion or laceration
(4) Tenderness
Explanation: According to the ACR Appropriateness Criteria, initial knee radiography may be appropriate in adults with acute knee trauma, such as a fall or twisting injury, especially when accompanied by clinical signs or symptoms. These include localized tenderness, swelling, joint effusion, or inability to bear weight. In the absence of such findings, routine initial imaging is generally not indicated. While superficial skin injuries alone (e.g., abrasions or lacerations) are not strong indicators, the presence of localized tenderness in this case makes initial radiography appropriate, even in the absence of high-energy trauma mechanisms.
2. Which of the following statements is TRUE regarding acute knee trauma in the emergency department?
(1) About 90% of radiographic findings do not correlate with clinical symptoms.
(2) Approximately 25% of patients demonstrate fractures on radiographs.
(3) Sprain injuries account for 75% of all knee injuries.
(4) All of the above.
Explanation: Approximately 5% of patients with acute knee trauma show fractures on plain radiographs. About 25% of findings on radiographs do not correlate with clinical symptoms. Twisting (sprain-related) injuries account for approximately 75% of all knee injuries, but 86% of knee fractures occur due to blunt trauma. Therefore, none of the listed choices is entirely accurate, and the correct answer should be: None of the above.
3. Patients with knee dislocation should undergo MRI in addition to initial radiography.
(1) True
(2) False
Explanation: If no fracture is evident on plain radiographs but there is suspicion of meniscal or ligamentous injury, or if there is concern for damage secondary to patellar dislocation, MRI is the most appropriate next step. In patients with knee dislocation, both radiographs and MRI are essential. Additional vascular imaging such as fluoroscopy, CT angiography, or MR angiography,y may also be necessary to assess for vascular injury.
CT Imaging:
Non-contrast axial and coronal images of the right knee.
Quiz 2
1. Which of the following findings is most likely in this case?
(1) Tibial plateau fracture
(2) Lipohemarthrosis
(3) Patellar tendon rupture
(4) All of the above
Explanation: Radiographs and CT images demonstrate an abnormal joint effusion with a superficial fat layer and a deeper blood layer within the suprapatellar region, indicative of marked lipohemarthrosis. No tibial plateau fracture is identified. Additionally, a subtle inferior patellar margin is visible on radiographs, which would likely not be seen in the case of a patellar tendon rupture.
2. Lipohemarthrosis is often indicative of an intra-articular fracture.
(1) True
(2) False
Explanation: The presence of a fat-fluid level within the joint strongly suggests the presence of an intra-articular fracture, even if the fracture is not radiographically visible. Lipohemarthrosis occurs in approximately 40% of knee joint fractures.
Question 3:
On radiographic evaluation, lipohemarthrosis can only be visualized with horizontal beam radiographs.
(1) True
(2) False
Explanation: Fat floats above blood, so horizontal beam radiographs are ideal for detecting the fat-fluid interface characteristic of lipohemarthrosis. This positioning allows clear visualization of layering within the joint.
4. Which fracture site is most commonly associated with lipohemarthrosis?
(1) Tibial plateau
(2) Femoral groove
(3) Femoral condyle
(4) Patella body
Explanation: Tibial plateau fractures are the most commonly associated injuries with lipohemarthrosis, followed by fractures of the femur and, less commonly, the patella. Importantly, approximately 60% of tibial plateau fractures may present only with hemarthrosis, without visible fat-fluid levels, so the absence of lipohemarthrosis does not exclude an intra-articular fracture.
5. Which of the following radiographic signs is indicative of lipohemarthrosis?
(1) FBI sign (Fat-Blood Interface)
(2) Parfait sign
(3) Double fat-fluid level
(4) All of the above
Explanation: Lipohemarthrosis refers to the presence of intra-articular fat and blood that separate into distinct layers following a fracture involving the bone marrow. The classic imaging hallmark is the FBI sign (Fat-Blood Interface), which reveals a clear horizontal layering with fat floating atop and blood settling below. In some cases, a hematocrit effect may be observed, where red blood cells sink beneath the serum, creating a two-layered fluid level that should not be mistaken for true lipohemarthrosis. When all three components—fat, serum, and red blood cells—form visible stratification, the condition is termed lipohydrohemarthrosis, also known as the Parfait sign due to its layered appearance. In patients with a well-developed suprapatellar plica, a double fat-fluid level may occasionally be detected on imaging.
6. Besides radiography, CT, MRI, and ultrasound are effective modalities for evaluating lipohemarthrosis.
(1) True
(2) False
Explanation: While radiographs are the most commonly used initial modality, CT, MRI, and ultrasound can all effectively identify lipohemarthrosis. CT offers a high-resolution depiction of fat-fluid levels, MRI is highly sensitive for marrow fat and soft tissue injuries, and ultrasound can occasionally detect layering fluid within the joint.
Differential Diagnosis
-
Traumatic fracture
-
Hemarthrosis
-
Osteonecrosis
-
Lipohemarthrosis
Diagnosis: Lipohemarthrosis
Pathophysiology
Lipohemarthrosis refers to the presence of fat and blood within a joint cavity, typically following intra-articular injury. It results from the extrusion of medullary fat into the synovial space, usually due to:
-
Occult intra-articular fractures (most commonly tibial plateau fractures), or
-
Extensive intra-articular soft tissue injuries
Key features of the pathophysiology include:
-
Medullary fat leaks into the joint space through a fracture line or damaged bone cortex
-
Fat rises above the blood within the joint cavity due to differences in specific gravity
-
It may become visible on imaging up to 3 hours post-trauma
Common fracture associations:
-
Most common: Tibial plateau
-
Others: Tibial spine, distal femoral condyle, patellar fracture (rare)
Complication:
-
Compartment Syndrome: A surgical emergency caused by elevated pressure within a closed fascial compartment, impairing perfusion and leading to ischemia or necrosis. Most commonly affects the lower leg (calf) or forearm.
Epidemiology
-
Most often identified in traumatic knee injuries, especially with increased use of horizontal beam radiography
-
Also seen in intra-articular fractures of the hip, shoulder, elbow, and wrist
-
Occurs in 35–41% of patients with traumatic knee injury
-
Up to 65% of patients with intra-articular fractures may not show fat-fluid levels on conventional radiographs
Clinical Presentation
-
Acute knee pain following trauma
-
Swelling and joint effusion
-
Inability to bear weight
Imaging Findings
Modalities:
-
Horizontal beam radiography
-
CT
-
MRI
Radiographic signs:
-
Fat-fluid level within the suprapatellar pouch, also known as the FBI sign (Fat-Blood Interface)
-
In cases with hematocrit effect, three fluid layers (fat, serum, and red blood cells) may be seen, referred to as the Parfait sign
-
In patients with a prominent suprapatellar plica, a double fat-fluid level may be observed
-
Associated fractures or soft tissue injuries may be subtle; 21% of fractures may be missed on initial radiographs, necessitating further evaluation
Ultrasound Features
-
Hypoechoic or anechoic joint effusion
-
Hyperechoic superficial layer representing fat above the blood/fluid
-
Useful in evaluating the suprapatellar pouch, particularly in resource-limited or point-of-care settings
Management
Conservative treatment:
-
Observation in stable cases
-
Joint aspiration (arthrocentesis) if indicated (e.g., pain relief, diagnostic clarification)
Surgical intervention:
-
Required for displaced intra-articular fractures,
-
Extensive soft tissue injuries, or
-
Recurrent joint effusions from severe trauma
References
- Bailey, M. A., Smith, M. P., & Orr, J. D. (2013). Lipohaemarthrosis: prevalence and diagnostic value in radiologically occult knee fractures. European Journal of Radiology, 82(10), 1692–1695. https://doi.org/10.1016/j.ejrad.2013.05.019
- Hunter, T. B., & Pyle, J. (2001). Musculoskeletal imaging: the relevance of fat–fluid levels. Radiographics, 21(3), 781–790. https://doi.org/10.1148/radiographics.21.3.g01ma06781
- Feller, J. F., & Bone, M. D. (1997). MR imaging of lipohemarthrosis: a potentially overlooked clue to intra-articular fracture. American Journal of Roentgenology, 169(5), 1419–1423. https://doi.org/10.2214/ajr.169.5.9353457
- Tang, L., Dai, K., & Wang, C. (2011). The role of imaging in the diagnosis and management of tibial plateau fractures. Injury, 42(10), 1118–1125. https://doi.org/10.1016/j.injury.2010.07.001
- Major, N. M., & Helms, C. A. (2002). Fat-fluid levels in lipohemarthrosis: a review. Radiology Clinics of North America, 40(5), 1045–1056. https://doi.org/10.1016/S0033-8389(02)00033-3





Comments
Post a Comment