Urachal duct cyst
1. Cause and Etiology
The urachus is a tube-like structure that connects the
bladder to the umbilicus in the fetus, facilitating the drainage of fetal
urine. In normal development, this structure closes off after birth, leaving a
fibrous cord, known as the median umbilical ligament. If the urachus fails to close
completely, various urachal anomalies may occur, including:
·
Urachal cyst: A
cyst forms when a portion of the urachal structure remains patent.
·
Urachal sinus: A
small opening remains at the umbilicus or bladder, allowing urine drainage.
·
Urachal fistula: A
patent channel between the bladder and the umbilicus remains open, allowing
urine to leak from the umbilicus.
The exact cause of
incomplete closure of the urachus is often unknown, but genetic factors, fetal
developmental abnormalities, or environmental influences may contribute.
2. Pathophysiology
·
During fetal development, the
urachus serves as a conduit for the elimination of fetal urine into the
amniotic sac.
·
Normally, after birth, the
urachus closes and becomes fibrous. However, if it does not close properly, a
cyst may form along the patent part of the urachus.
·
The cyst is usually lined by
transitional epithelium, which is characteristic of the urinary tract, and can
be filled with mucinous or serous fluid.
·
Over time, if the cyst becomes
infected, it may lead to inflammation and symptoms such as abdominal pain,
fever, or even abscess formation.
3. Epidemiology
·
Incidence: Urachal
duct cysts are rare, occurring in approximately 1 in 5,000 to 1 in 40,000 live births.
·
Age of Presentation: Most cases are diagnosed in childhood or adolescence, but they can
also present in adults. The symptoms may not appear until the cyst enlarges or
becomes infected, often leading to delayed diagnosis.
·
Sex Distribution:
There is a slight male predominance for urachal abnormalities, but cysts
themselves are generally not sex-specific.
·
Associations:
Urachal duct cysts can occasionally be associated with other urological
anomalies, such as bladder exstrophy or epispadias.
4.
Clinical Presentation
Urachal duct cysts may be asymptomatic, especially when
small. However, as they enlarge or become infected, they can cause a range of
symptoms:
·
Abdominal Pain:
Localized pain or discomfort, particularly in the lower abdomen, often near the
umbilicus or above the pubis.
·
Urinary Symptoms:
Dysuria, hematuria, or urinary tract infections may be seen if the cyst
communicates with the bladder or if infection sets in.
·
Palpable Mass: A
soft, non-tender mass may be palpable in the lower abdomen, especially in the
midline.
·
Infection Symptoms:
Fever, chills, and erythema over the cyst or nearby skin if the cyst becomes
infected.
·
Umbilical Discharge: If the cyst communicates with the umbilicus (through a urachal
sinus), it may present with a mucoid or purulent discharge.
5. Imaging Features
Several imaging modalities can be used to diagnose a
urachal duct cyst:
·
Ultrasound (US):
The first-line imaging tool. The cyst typically appears as a well-defined
anechoic or hypoechoic structure in the lower abdomen near the bladder, often
above the pubis. Doppler can help assess blood flow around the lesion.
·
Computed Tomography (CT): A CT scan provides detailed information about the cyst's size, location, and relationship to surrounding structures. It can also help
identify complications like infection or abscess formation.
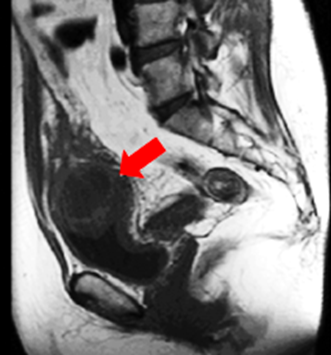
·
Magnetic Resonance Imaging (MRI): MRI offers excellent soft tissue contrast and can delineate the
cyst’s boundaries, especially concerning surrounding tissue
involvement or infection.
6. Treatment
Treatment strategies depend on the severity of the symptoms
and the risk of complications:
·
Asymptomatic Urachal Cyst: If the cyst is small and asymptomatic, it may be managed
conservatively with observation, especially if there are no signs of infection
or other complications.
·
Infected Cyst: If
the cyst becomes infected, antibiotics are often required to treat the
infection. If abscess formation occurs, surgical drainage may be necessary.
·
Surgical Excision:
The definitive treatment for symptomatic or complicated urachal cysts (such as
recurrent infection or large cysts) is surgical excision. The procedure
involves complete removal of the cyst, including any remnant urachal tissue, to
prevent recurrence.
·
Fistula or Sinus:
If a urachal fistula or sinus is present, surgical repair is needed to close
the communication between the bladder and the umbilicus.
7. Prognosis
·
With Treatment:
After surgical excision, the prognosis is generally excellent, with low
recurrence rates. Complications such as infection or abscess formation can be
effectively managed with antibiotics and drainage.
·
Without Treatment:
If left untreated, complications such as recurrent infections, chronic
abdominal pain, or the formation of bladder stones may occur. In rare cases,
malignancy (urachal carcinoma) can develop from the urachal remnant in later
life, though this is extremely uncommon.
Long-term Prognosis: After successful removal of the cyst, patients can lead normal lives without significant long-term issues, assuming no further complications arise.
Conclusion
A urachal duct cyst is a rare but treatable condition, primarily arising due to incomplete closure of the urachus after birth. It can present with a variety of symptoms, most commonly abdominal pain or a palpable mass. Imaging techniques, especially ultrasound, help in diagnosis. The treatment of choice is surgical excision, which offers an excellent prognosis in the majority of cases.



Comments
Post a Comment