Talc Pleurodesis
1. Cause / Purpose of Talc Pleurodesis
Talc pleurodesis is not a disease, but a therapeutic medical
procedure used to obliterate the pleural space to prevent recurrent
pleural effusions or pneumothoraces. It involves the instillation of
sterile talc powder into the pleural space to induce inflammation and
fibrosis, resulting in adhesion of the visceral and parietal pleura.
Common indications:
- Malignant
pleural effusion (most
common)
- Recurrent
pneumothorax
- Chylothorax
- Refractory
benign pleural effusions
2. Etiology
Since talc pleurodesis is a deliberately induced condition, its
"etiology" refers to why and how it is performed, rather than
a natural cause. The etiological rationale is:
- Mechanical prevention of
pleural fluid or air reaccumulation.
- Symptomatic relief (e.g.,
dyspnea).
- Improved quality of life
in palliative care settings.
Talc is the agent of choice due to:
- High efficacy
- Low cost
- Broad availability
- Minimal systemic
absorption
3. Pathophysiology
Talc pleurodesis causes intentional pleural inflammation and fibrosis:
- Talc
particles (preferably
large-particle, asbestos-free, medical-grade) are insufflated or instilled
into the pleural space.
- These particles cause local
irritation, leading to:
- Activation of
mesothelial cells
- Release of proinflammatory
cytokines (e.g., IL-8, TNF-α, TGF-β)
- Neutrophil
and macrophage infiltration
- This cascade results in exudative
pleuritis and fibrous adhesion between the parietal and
visceral pleura.
- Permanent
pleural symphysis obliterates
the pleural space, thereby preventing further fluid or air accumulation.
The degree of inflammation depends on:
- Talc particle size
(smaller particles increase systemic dissemination and side effects)
- Dose
- Patient’s immune status
4. Epidemiology
Since talc pleurodesis is procedural:
- Its “epidemiology”
depends on the underlying condition (e.g., pleural malignancy).
- Used commonly in oncology
and pulmonology.
Malignant pleural effusion (MPE):
- Occurs in ~15% of all
cancer patients.
- Common in lung cancer,
breast cancer, ovarian cancer, mesothelioma, and lymphoma.
- Talc pleurodesis is one
of the most frequently used interventions in the palliative care of
MPE.
Pneumothorax:
- Spontaneous pneumothorax
recurrence rates are ~30-50%.
- Talc pleurodesis is used
especially in patients not fit for surgery or with recurrence.
5. Clinical Presentation
Since talc pleurodesis is a treatment, the clinical “presentation”
refers to post-procedural symptoms or complications:
Expected post-procedural symptoms:
- Chest pain (common, due to inflammation)
- Fever
- Dyspnea (transient, typically improves after fluid
resolution)
Complications:
- Acute respiratory distress
syndrome (ARDS) (rare; more likely with small-particle talc)
- Empyema
- Fever of unknown origin
- Hypoxemia
- Pneumonitis (especially
with talc of non-uniform particle size)
- Acute pain requiring
opioids
6. Imaging Features
Chest X-ray (CXR):
- Immediate
post-pleurodesis: pleural thickening, homogeneous opacity,
residual fluid.
- Later stages: calcified
pleura (in some cases).
CT Findings:
- High
attenuation pleural lining (due to
talc deposition; >80 HU)
- Diffuse
pleural thickening with
increased enhancement
- Pleural
nodularity (must differentiate from
malignant pleural disease)
- Persistent talc may mimic
pleural metastasis—clinical history is essential.
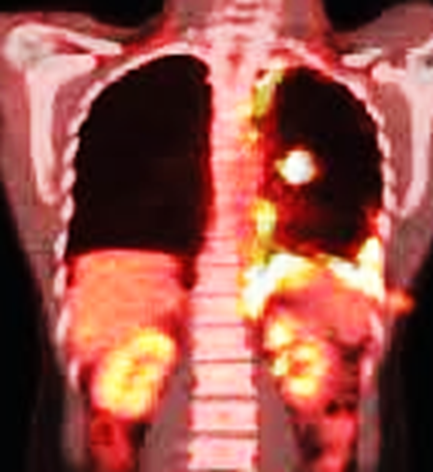
PET-CT:
- Talc can cause increased
FDG uptake, mimicking malignancy.
- Uptake may persist for
months or years, especially in areas of inflammation.
Radiological Pearls:
·
Always correlate
with a clinical history of pleurodesis.
·
Distinguish from mesothelioma,
empyema, or recurrent malignancy.
7. Treatment Strategy
Talc pleurodesis is both diagnostic and therapeutic.
Talc can be administered via:
- Thoracostomy
(tube thoracostomy) with slurry
- Thoracoscopy
(VATS or medical thoracoscopy) with poudrage (spray insufflation)
Key Steps:
- Drain the pleural fluid
completely.
- Ensure full lung
expansion.
- Instill sterile talc
slurry via chest tube OR insufflate talc powder under thoracoscopic
guidance.
- Clap chest tube for 1–2
hours to facilitate contact.
- Unclamp and monitor
drainage.
Contraindications:
- Trapped lung
(unexpandable lung)
- Active infection
(empyema)
- Severe coagulopathy
- Allergy to talc (rare)
8. Prognosis and Efficacy
Success rate:
- Varies from 70–90%,
higher when performed thoracoscopically.
- Talc poudrage (via thoracoscopy) may have better outcomes than
slurry.
Factors affecting outcome:
- Lung expansion capacity
- Presence of malignancy
- Inflammatory response
Long-term outlook:
- Permanent pleural
adhesion in most patients.
- Symptom relief (dyspnea)
is the main goal.
- In malignant effusion,
part of palliative care, not curative.
Complications and Prognosis:
- Serious complications
(e.g., ARDS) are rare with large-particle talc.
- Persistent pleural
thickening may limit future thoracic procedures.
- In terminal cancer, it improves quality of life but does not affect survival.
Chest X-ray Report (Post-Pleurodesis)
Indication:
Follow-up imaging post-pleurodesis for malignant pleural effusion.
Findings:
There is evidence of pleural thickening in the right
hemithorax, consistent with post-pleurodesis changes. No pneumothorax is seen.
The lung appears fully expanded. No significant pleural effusion is currently
evident. No acute osseous abnormality. The heart and mediastinum are within normal
limits.
Impression:
Stable post-talc pleurodesis changes. No evidence of recurrent effusion or
pneumothorax.
Case study: A 69-Year-Old Male with Right Flank Pain
Talc Pleurodesis
History and Imaging Findings
-
A 69-year-old male presented with complaints of right flank pain.
-
No respiratory symptoms were reported.
-
The patient had a history of recurrent left-sided lung collapse and had undergone thoracic surgery on the left side several years prior.
-
Non-contrast-enhanced abdominal CT was performed, capturing both axial and reformatted sagittal views of the lower thorax. Imaging was reviewed in both soft tissue (upper panels) and lung window settings (lower panels).
-
No radiologic evidence of urolithiasis was identified.
Quiz
-
What is the most significant finding on the CT scan?
(1) Nodular pleural thickening with calcifications
(2) Left-sided rib fractures
(3) Right pleural effusion
(4) Aortic dissection -
Which of the following are included in the differential diagnosis of nodular pleural thickening?
A. Primary pleural malignancy
B. Metastatic disease
C. Talc pleurodesis
D. A, B, and C
E. None of the above -
What are the typical indications for talc pleurodesis?
A. Recurrent pneumothorax
B. Recurrent pleural effusion
C. Both A and B
D. Neither A nor B -
Talc pleurodesis functions by inducing adhesion between the parietal pleura and the chest wall.
(1) True
(2) False
Explanation: Talc pleurodesis works by promoting adhesion between the parietal and visceral pleura. -
Talc deposits demonstrate FDG avidity on F-18 FDG PET/CT.
(1) True
(2) False
Explanation: Intense FDG uptake due to granulomatous inflammatory response can persist for decades.
Findings and Diagnosis
Findings
Non-contrast-enhanced CT reveals irregular, hyperdense soft tissue thickening along the multifocal surfaces of the left pleura, with subtle calcifications (red arrows). These findings are consistent with prior talc pleurodesis.
Differential Diagnosis
-
Mesothelioma
-
Pleural metastasis
-
Talc pleurodesis
-
Granulomatous infection
Final Diagnosis:
Talc pleurodesis
Discussion
Talc Pleurodesis
Pathophysiology and Epidemiology
Chemical pleurodesis is a therapeutic procedure performed to prevent recurrent pneumothorax or pleural effusion.
Instillation of talc between the pleural surfaces induces intense intrapleural inflammation and subsequent fibrosis.
This fibrotic reaction leads to adhesion between the visceral and parietal pleura.
The procedure has a reported success rate exceeding 90%.
Clinical Presentation
Patients are generally asymptomatic.
Post-procedural complications may include fever and gastrointestinal symptoms shortly after instillation.
Imaging Characteristics
-
CT: Nodular or linear pleural thickening with variable degrees of calcification. The findings are expected to remain stable over serial imaging.
-
F-18 FDG PET/CT: FDG avidity may be observed in areas of pleural thickening resulting from talc pleurodesis.
Management
-
Long-term adverse effects from talc pleurodesis are minimal.
-
Symptom control is the main focus immediately following the procedure.
(1) Baiu
I, Yevudza E, Shrager JB. Talc pleurodesis: A medical, medicolegal, and
socioeconomic review. Ann Thorac Surg. 2020;109(4):1294-1301.
(2) Narayanaswamy
S, Kamath S, Williams M. CT appearances of talc pleurodesis. Clin Radiol.
2007;62(3):233-237.
(3) Peek
H, van der Bruggen W, Limonard G. Pleural FDG uptake more than a decade after
talc pleurodesis. Case Rep Med. 2009;2009:650864.





Comments
Post a Comment