Superficial thrombophlebitis of the cephalic vein-A 52-Year-Old Woman with Right Arm Swelling and Redness
Superficial thrombophlebitis of the cephalic vein
1. Cause and Etiology
Superficial thrombophlebitis (STP) of the cephalic vein occurs when there is inflammation and thrombus
(blood clot) formation within the cephalic vein, a superficial vein located
along the lateral (thumb) side of the upper limb.
Common causes and risk factors include:
- Venous
cannulation or intravenous (IV) lines: Insertion of catheters into the cephalic vein is a major
precipitating event.
- Trauma or
irritation: Mechanical injury
during venipuncture, blood draws, or trauma.
- Hypercoagulable
states: Inherited
thrombophilias (e.g., Factor V Leiden mutation, protein C/S deficiency),
malignancy, pregnancy, or estrogen therapy.
- Infection: Local or systemic infections can promote
endothelial damage and thrombosis.
- Inflammatory
diseases, Such as Behçet’s
disease or Buerger’s disease.
- Prolonged
immobilization: Less common
for superficial veins, but still possible.
- Varicose
veins: More relevant in the lower
limbs, but superficial venous disease predisposes to thrombophlebitis in
general.
2. Pathophysiology
The underlying process follows Virchow’s triad:
- Endothelial
injury: Trauma from IV lines or
blood draws causes endothelial disruption, promoting clot formation.
- Venous stasis: Immobility or compression around the vein slows
blood flow.
- Hypercoagulability: Systemic or local prothrombotic conditions
enhance clotting.
When these factors converge:
- Endothelial cells
activate platelets and the coagulation cascade.
- A thrombus forms within the
vein lumen.
- Inflammatory cells
(neutrophils, macrophages) infiltrate the vessel wall.
- Vein becomes inflamed,
thickened, tender, and often cord-like.
Secondary infection (septic thrombophlebitis) can complicate the condition,
especially if IV lines were involved.
3. Epidemiology
- Age: More common in adults, especially middle-aged
and elderly.
- Gender: Slight female predominance (possibly related to
hormone use and varicosities).
- Incidence: Exact rates for cephalic vein-specific
thrombophlebitis are unclear, but STP in general is a relatively frequent
vascular condition, especially in hospitalized patients with IV catheters.
- Risk settings: Hospitalization, IV drug use, cancer, and autoimmune
diseases.
4. Clinical Presentation
Patients typically present with:
- Localized
pain over the cephalic vein in
the forearm or upper arm.
- Erythema and
swelling along the course of the
vein.
- Palpable cord: A firm, tender vein can often be felt under the
skin.
- Warmth over the area.
- Minimal
systemic symptoms: Fever is
rare unless infection complicates the thrombophlebitis.
- Reduced range
of motion: Particularly if the
inflammation is extensive.
- No
significant limb edema: Unlike deep
vein thrombosis (DVT).
In cases with septic thrombophlebitis:
- Fever, chills, and
purulent drainage may be present.
5. Imaging Features
Ultrasound with Doppler is the imaging
modality of choice:
- Non-compressibility of the cephalic vein.
- Intraluminal
echogenic material consistent
with thrombus.
- Absence of
normal venous flow on color
Doppler.
- Perivascular
inflammatory changes: Soft tissue
edema around the vein.
- Wall
thickening: Sometimes seen.
- No extension
into deep veins: Important
to differentiate from DVT.
Rarely, MRI or CT may be used if there is concern about extension,
mass effect, or infection.
6. Treatment
Most cases are self-limited and can be treated conservatively:
- Local
measures:
- Warm compresses.
- Limb elevation.
- Nonsteroidal
anti-inflammatory drugs (NSAIDs) for pain and inflammation.
- Anticoagulation:
- Usually not required
unless:
- The
thrombosis is near the deep venous system (e.g., at the axillary vein
junction).
- The
thrombosis is extensive.
- A patient has
hypercoagulable risk factors.
- If anticoagulation is
used, low-molecular-weight heparin (LMWH) or direct oral anticoagulants
(DOACs) may be prescribed.
- Antibiotics:
- Only if septic
thrombophlebitis is suspected (e.g., fever, purulence).
- Surgical
intervention:
- Rarely needed.
- Thrombectomy or vein
ligation may be considered if there is extensive clot, progression
despite treatment, or a septic focus.
- Removal of
offending IV line or catheter:
- Essential if
thrombophlebitis is related to cannulation.
7. Prognosis
- Excellent
prognosis in uncomplicated cases.
- Symptoms typically
resolve within 1–2 weeks.
- Recurrence is rare if
risk factors are addressed.
- Complications are
uncommon but may include:
- Extension into deep
veins (DVT).
- Pulmonary embolism
(extremely rare in isolated cephalic vein thrombosis).
- Chronic venous
insufficiency (rare).
- Septicemia occurs if the infection
spreads.
Follow-up is necessary if:
- Symptoms worsen.
- There are signs of DVT or
systemic infection.
- A patient has ongoing
prothrombotic risk factors.
Case study: A 52-Year-Old Woman with Right Arm Swelling and Redness Superficial Thrombophlebitis of the Cephalic Vein
History and Imaging
-
A 52-year-old woman with a history of multiple malignancies, including oropharyngeal carcinoma, presented with swelling and redness of the right arm following a recent hospital discharge.
-
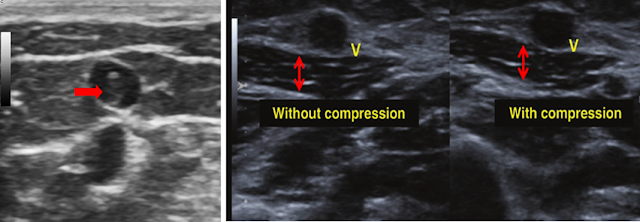
Multiple images of the distal radial vein were obtained using B-mode, M-mode ultrasound, and color Doppler. Comparative images of the proximal axillary vein were also provided, including compression views.
Quiz:
-
What is the most prominent abnormal finding?
(1) Superficial thrombophlebitis of the axillary vein
(2) Deep venous thrombosis
(3) Superficial thrombophlebitis of the cephalic vein
(4) Post-thrombotic syndrome -
What is the greatest risk factor for this condition?
(1) Female sex
(2) Male sex
(3) Age under 60 years
(4) Use of anticoagulation medication -
Which group has the highest risk of complications from this condition?
(1) Males
(2) Females
(3) Individuals under 60 years old
(4) Those taking anticoagulant medication -
Which vessel is most associated with a higher risk of complications in this condition?
(1) Cephalic vein
(2) Basilic vein
(3) Greater saphenous vein
(4) Radial vein
Findings and Diagnosis
Findings
Ultrasound examination revealed that the superficial branches of the distal right cephalic vein were dilated and heterogeneous, showing diminished and turbulent flow.
Differential Diagnosis
-
Deep vein thrombosis (DVT)
-
Post-thrombotic syndrome
-
Thrombophlebitis
-
Phlegmasia
-
Cellulitis
Diagnosis: Superficial thrombophlebitis of the cephalic vein
Discussion
Superficial Thrombophlebitis of the Cephalic Vein
Superficial thrombophlebitis is an inflammatory process associated with thrombus formation within a superficial vein. Traditionally, it has been considered a benign and self-limiting condition. Although there have been claims suggesting that superficial thrombophlebitis may be associated with deep vein thrombosis (DVT), this remains controversial.
Epidemiology
The incidence of superficial thrombophlebitis is not well studied but is thought to be higher than that of deep vein thrombosis, which occurs in approximately 1 in 1,000 people annually. It is more common in elderly patients and females; however, males are more likely to develop complications. Thrombosis involving the greater saphenous vein is most strongly associated with an increased risk of complications.
Clinical Presentation
-
Pain, redness, and swelling over the area of thrombosis
Imaging Features
-
Non-compressible vein
-
Presence of intraluminal thrombus in the affected vein
-
Reduced venous pulsatility
-
Lack of vein expansion during the Valsalva maneuver
-
Loss of Doppler flow signal
Treatment
The treatment of superficial thrombophlebitis primarily involves the use of anticoagulation. Although evidence is limited, fondaparinux has the strongest supporting data. The main goals of treatment are to relieve local symptoms and to prevent extension of the thrombus into the deep venous system. However, the overall quality of evidence is low due to limitations in study design.
References
(1) Decousus
H, Epinat M, Guillot K, Quenet S, Boissier C, Tardy B. Superficial vein thrombosis:
Risk factors, diagnosis, and treatment. Curr Opin Pulm Med. 2003;9(5):393-397.
(2) Di
Nisio M, Wichers IM, Middeldorp S. Treatment for superficial thrombophlebitis
of the leg. Cochrane Database Syst Rev. 2018;2(2): CD004982. doi:
10.1002/14651858.CD004982.pub6.
(3) Lutter
K, Kerr T, Roedersheimer L, Lohr J, Sampson M, Cranley J. Superficial
thrombophlebitis diagnosed by duplex scanning. Surgery. 1991;110(1):42-46.
(4) Nasr
H, Scriven J. Superficial thrombophlebitis (superficial venous thrombosis).
BMJ. 2015;350:h2039. doi: 10.1136/bmj.h2039.
(5) Ploton
G, Pistorius MA, Raimbeau A, et al. A STROBE cohort study of 755 deep and
superficial upper-extremity vein thrombosis. Medicine (Baltimore).
2020;99(6):e18996. doi: 10.1097/MD.0000000000018996.


Comments
Post a Comment