Branchial cleft cyst
A branchial cleft cyst is a congenital lesion that arises from the branchial arches during embryonic development. It typically manifests as a soft, painless mass in the neck.
Cause & Etiology:
Branchial cleft cysts develop as a result of incomplete closure or
involution of the branchial apparatus (a structure involved in the development
of the neck and associated structures). The branchial apparatus is composed of
branchial arches, clefts, pouches, and membranes.
The cysts arise from:
- 1st Branchial
Cleft: The most common origin,
leading to cysts located near the angle of the mandible.
- 2nd Branchial
Cleft: The most frequent site for
branchial cleft cysts (around the anterior border of the
sternocleidomastoid muscle).
- 3rd and 4th
Branchial Clefts: Rare, but
these cysts can be located in deeper neck structures, possibly around the
thyroid or near the trachea.
The cause of incomplete closure is typically unknown but can be linked to
genetic factors or disturbances during fetal development.
Pathophysiology:
The branchial cleft cyst forms when remnants of the branchial cleft fail
to fully regress during fetal development. Instead of being reabsorbed or
incorporated into the surrounding tissues, the remnants become fluid-filled
cystic structures. These cysts remain as isolated, epithelial-lined spaces that
may or may not become infected.
The cyst is usually filled with clear or serous fluid, and its lining
consists of squamous or columnar epithelium. Infection can cause enlargement,
pain, and potential rupture.
Epidemiology:
- Incidence: These cysts are rare, accounting for about 20%
of all congenital neck masses.
- Age of
Presentation: Most
commonly, branchial cleft cysts are diagnosed in children or young adults,
often presenting between the ages of 2-4 years.
- Sex: There is no significant difference in the
incidence between males and females.
- Laterality: Affected individuals often present with cysts
on one side, though bilateral cases can occur, particularly with the 2nd
branchial cleft cyst.
Clinical Presentation:
- Neck Mass: The most common presenting symptom is a
painless, firm, smooth mass in the neck, often along the anterior or
lateral aspect of the sternocleidomastoid muscle (SCM).
- Size: It can vary in size and may fluctuate over
time, particularly with infection.
- Infection: When infected, the cyst may become tender, red,
and warm to the touch. There may also be drainage of pus or serous fluid.
- Symptoms of
Inflammation: Fever,
local erythema, and swelling may accompany infection.
- Difficulty
Swallowing: Rarely, the cyst can
cause difficulty swallowing if it presses on the esophagus or other
structures.
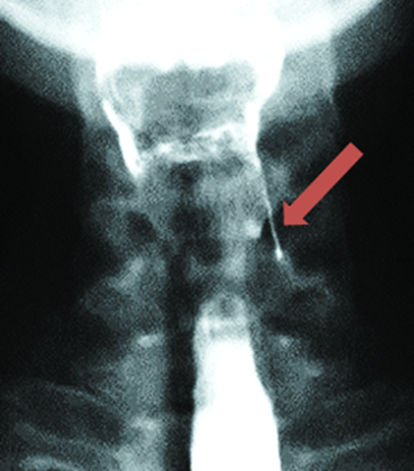
Imaging Features:
- Ultrasound: Commonly used as an initial imaging technique
to distinguish cystic masses from solid masses. It shows a well-defined,
anechoic (fluid-filled) structure with regular borders.
- CT Scan: More detailed imaging for larger cysts or when
complications are suspected. It shows a smooth, fluid-filled lesion with
minimal enhancement if non-infected.
- MRI: Particularly helpful for evaluating the cyst's
relationship to surrounding structures and for determining the exact
origin of the cyst. A branchial cleft cyst typically appears as a
well-defined, round or oval mass, with homogenous fluid signal.
- Contrast
Enhanced Imaging: May show
enhancement if the cyst is infected or inflamed.
Treatment:
The mainstay of treatment for a branchial cleft cyst is surgical
excision. The goals are to:
- Remove the cyst
completely to prevent recurrence.
- Avoid injury to
surrounding vital structures such as nerves (e.g., facial nerve, vagus
nerve), blood vessels, and muscles.
Specific Treatment Considerations:
- Infection: If the cyst becomes infected, it is usually
managed with antibiotics first. If the infection does not resolve or if
the cyst is severely infected, surgical drainage or excision may be
required.
- Non-Infected
Cysts: These are typically
excised electively, especially if they cause cosmetic concerns or are
growing in size.
Prognosis:
- Post-Surgical
Outcome: If fully excised, the
prognosis is excellent, with a very low recurrence rate.
- Infection
Complications: If the cyst
becomes infected and drainage or excision is delayed, there could be an
increased risk of recurrence or complications such as abscess formation or
fistula development.
- Recurrence: Recurrence can occur if the cyst is
incompletely excised or if there are remnants left behind.
Key Points:
- Branchial
cleft cysts are typically congenital
and are most commonly found along the 2nd branchial arch.
- Surgical
excision is the definitive
treatment, with a good prognosis if complete removal is achieved.
- Early identification and appropriate management can prevent complications like infection or recurrence.



Comments
Post a Comment