Arachnoid Cysts
1.
Cause and Etiology
Arachnoid cysts are cerebrospinal fluid (CSF)-filled sacs
that occur within the arachnoid membrane, which is one of the three meningeal
layers that surround the brain and spinal cord. The etiology is broadly
categorized into:
A. Primary (Congenital)
Arachnoid Cysts
·
These are by far the most
common type.
·
Result from developmental abnormalities
during embryogenesis, especially between the 3rd and 4th months
of gestation.
·
It is thought to be caused by splitting or duplication
of the arachnoid membrane, leading to a CSF-filled pocket.
B. Secondary (Acquired)
Arachnoid Cysts
·
Less common.
·
Typically result from:
o
Head trauma
o
Infections (e.g., meningitis)
o
Intracranial hemorrhage
o
Surgical complications
o
Neurosurgical interventions
2.
Pathophysiology
·
Arachnoid cysts are lined by flattened arachnoid cells
or mesothelial-like
cells and contain CSF or CSF-like fluid.
·
They are not in communication with the
ventricular system, although some may develop secondary
communication over time.
·
The exact mechanism of cyst
enlargement is not fully understood, but proposed mechanisms include:
o
Active fluid secretion by the cyst wall.
o
Osmotic gradient
draws fluid into the cyst.
o
One-way ball-valve mechanism allowing CSF to enter but not exit.
These cysts may cause mass effect on adjacent brain
tissue, leading to neurological symptoms depending on size and location.
3.
Epidemiology
·
Estimated prevalence: ~1-2% in the
general population.
·
Often detected incidentally
during neuroimaging for unrelated reasons.
·
Male predominance
(~2:1).
·
Congenital cysts are more
common in children
and young adults, while acquired cysts may present at any age.
·
Most common locations:
o
Middle cranial fossa (especially left side)
o
Cerebellopontine angle (CPA)
o
Suprasellar region
o
Quadrigeminal cistern
o
Convexities and spinal canal
4.
Clinical Presentation
Most arachnoid cysts are asymptomatic. When symptomatic,
clinical features are determined by the cyst’s location, size, and effect on surrounding
structures:
Neurological Symptoms
·
Headache (most
common symptom)
·
Nausea and vomiting (due to increased intracranial pressure)
·
Seizures
·
Cranial nerve deficits (if compressing cranial nerve pathways)
·
Hydrocephalus (if
CSF flow is obstructed)
·
Developmental delay or behavioral changes in children
·
Ataxia, hemiparesis, or other focal neurological
deficits
Spinal Arachnoid Cysts (rare)
·
Present with radiculopathy, myelopathy, or progressive motor weakness.
5.
Imaging Features
A. CT Scan
·
Well-defined, hypodense (low attenuation)
lesion.
·
Non-enhancing.
·
No calcification or hemorrhage
(unless complicated).
·
Adjacent bony remodeling or
thinning may be seen due to chronic pressure.
B. MRI (Modality of choice)
·
T1-weighted:
Hypointense (same as CSF)
·
T2-weighted:
Hyperintense (same as CSF)
·
FLAIR: Signal
suppressed (helps differentiate from epidermoid cysts, which are not
suppressed)
·
DWI: No restricted
diffusion (unlike epidermoid cysts)
·
No enhancement
after contrast administration.
C. Cine MRI (CSF Flow Study)
·
May show absence of
communication with the subarachnoid space.
D. Differential Diagnosis
·
Epidermoid cyst
·
Porencephalic cyst
·
Neuroglial cyst
·
Cystic tumors (e.g., pilocytic astrocytoma)
·
Hydrocephalus ex vacuo
6.
Treatment
Treatment decisions depend on symptoms, size, growth, and complications
such as hydrocephalus.
A. Conservative Management
·
Indicated for asymptomatic or minimally
symptomatic cases.
·
Includes serial imaging (MRI)
to monitor cyst growth or structural changes.
B. Surgical Management
Indicated for:
·
Progressive symptoms
·
Neurological deterioration
·
Raised intracranial pressure
·
Mass effect or hydrocephalus
Surgical
options:
1.
Microsurgical or Endoscopic Fenestration
o
Create a window between the
cyst and the adjacent subarachnoid space or ventricle.
o
Preferred in cysts with an accessible anatomic location.
2.
Cystoperitoneal Shunting
o
Drainage of cyst contents into
the peritoneal cavity using a catheter and valve system.
o
Reserved for inaccessible or
recurrent cysts.
3.
Complete Excision
o
Rare; only in cases where total
removal is feasible and safe.
4.
Spinal Cysts
o
Laminectomy and cyst
fenestration/excision.
7.
Prognosis
·
Generally excellent in
asymptomatic cases.
·
Surgical outcomes
are good, especially for accessible cysts with clear indications.
·
Recurrence may occur,
especially with incomplete fenestration.
·
Rare complications:
o
Hemorrhage into a cyst
o
Cyst rupture
o
Infection (after surgical
intervention)
Long-term monitoring is recommended post-surgery for
recurrence or new symptom development.
Summary
Table
|
Category |
Details |
|
Cause |
Congenital (common), Acquired (trauma,
infection, hemorrhage) |
|
Pathophysiology |
CSF-filled cyst between arachnoid layers;
mass effect; fluid accumulation mechanisms |
|
Epidemiology |
1–2% prevalence; male predominance;
mostly incidental |
|
Clinical Features |
Headache, seizures, hydrocephalus,
neurological deficits |
|
Imaging |
Hypodense on CT; CSF-like signal on MRI;
no enhancement |
|
Treatment |
Observation vs. surgical fenestration or
shunting |
|
Prognosis |
Good with or without surgery; recurrence is possible post-op |
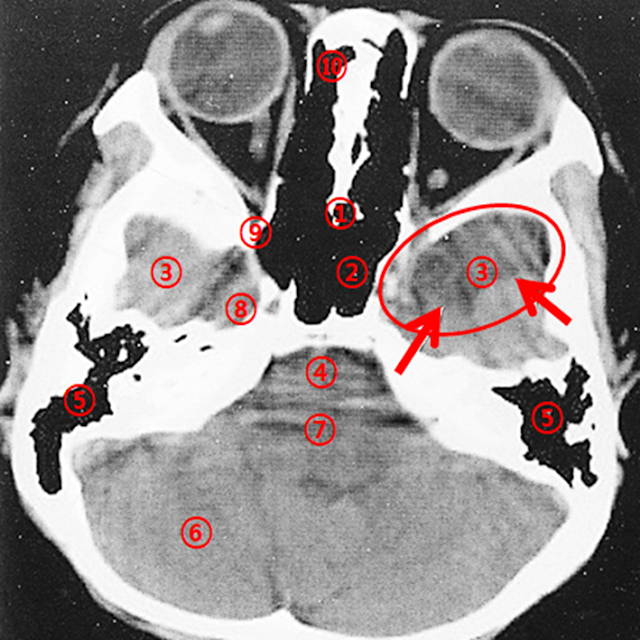
Axial Section Passing Through the Petrous Part of the
Temporal Bone
Case: A 10-year-old male with a well-defined Low Density Area (LDA)
observed in the left middle cranial fossa.
Normal Scan
Cerebral Palsy
Comparison Scan
A well-defined low-density area (LDA) is noted in the left middle cranial
fossa (red arrow). The sphenoid bone appears slightly thinned. These findings
are suggestive of an arachnoid cyst, which commonly occurs in the middle
cranial fossa. Although chronic infarction or contusion may be considered as
differential diagnoses, the thinning of the adjacent bone increases the
likelihood of an arachnoid cyst. Bone setting views can provide
additional diagnostic value.
Discussion: Arachnoid Cysts
An arachnoid cyst is a cerebrospinal fluid (CSF)-filled sac that develops
between the layers of the arachnoid membrane, one of the three meninges that
surround the brain and spinal cord. These cysts are most commonly congenital,
meaning they are present at birth and usually arise due to developmental
abnormalities during fetal growth. However, they may also be acquired
later in life as a result of head trauma, infection, or intracranial
hemorrhage.
Arachnoid cysts are typically benign and often asymptomatic,
frequently discovered incidentally during neuroimaging performed for unrelated
reasons. Nonetheless, in some cases, particularly when the cyst enlarges or
exerts pressure on adjacent brain structures, they may lead to symptoms or
complications. Common symptoms associated with arachnoid cysts include:
- Headaches: Persistent headaches, especially when
intracranial pressure is elevated.
- Nausea and
Vomiting: Possibly due to increased
intracranial pressure.
- Seizures: Arachnoid cysts may disrupt normal brain
function, resulting in seizures.
- Hydrocephalus: In some instances, the cyst may obstruct CSF
flow, causing hydrocephalus—a condition characterized by fluid
accumulation in the cerebral ventricles.
- Behavioral
Changes: Particularly in
children, irritability, mood swings, and other behavioral disturbances may
be observed.
- Motor or
Sensory Deficits: Depending
on the cyst’s location and size, compression of adjacent brain tissues may
result in weakness, numbness, or other neurological deficits.
Treatment depends on factors such as
cyst size and location, severity of symptoms, and the individual’s overall
health status. In many cases, conservative management with regular
imaging follow-up is sufficient, particularly if the cyst is asymptomatic or
causes only mild symptoms. Surgical intervention may be indicated when the cyst
is symptomatic or leads to complications such as hydrocephalus. Surgical
options include:
- Cyst
Fenestration: Creating a
small opening in the cyst wall to allow drainage of CSF into the
subarachnoid space.
- Cyst Shunting: Insertion of a catheter to divert fluid from
the cyst to another body cavity, such as the peritoneal cavity.
It is essential for individuals with arachnoid cysts to receive comprehensive
care from a neurologist or neurosurgeon, who can monitor the condition and
recommend appropriate treatment strategies based on individual needs.
Case: A 4-year-old male with developmental delay
Poor development of the left mastoid air cells and the mastoid
antrum demonstrates soft-tissue density instead of air (arrow). These
findings raise suspicion of chronic otitis media.
The sphenoethmoidal sinus is underdeveloped (arrow). When mastoid
air cells appear opaque on imaging, it may be due either to hypoplasia
(as seen in chronic otitis media) or to fluid or secretions retention
(as seen in acute otitis media).
Differentiation between these
entities can be aided by utilizing bone setting views, which involve
increasing the window width and raising the window level for enhanced bone
visualization.
Advantages of CT Bone Setting
Compared to conventional techniques, CT bone setting offers several
benefits:
- Precision: CT imaging provides detailed visualization of
bony structures, facilitating accurate planning and execution of reduction
procedures.
- Customization: Virtual reconstruction allows personalized
treatment planning tailored to each patient’s unique anatomy and injury
pattern.
- Minimally
Invasive Approach: In some
cases, the use of CT-guided techniques enables less invasive procedures
compared to traditional surgeries, potentially reducing recovery time and
complication risks.
CT Imaging Parameters: Window Level and Window Width
In CT imaging, the terms "window level" (WL) and "window
width" (WW) refer to image processing parameters used to optimize the
visualization of specific tissues or structures within the scanned region.
- Window Level
(WL): Determines the center
value of the gray scale range displayed in the image. It primarily adjusts
the brightness of the image. Higher WL values make the image appear
brighter, while lower values darken the image. For example, a higher WL is
typically used for bone imaging, whereas lower WL values enhance
the visibility of soft tissues.
- Window Width
(WW): Defines the range of CT
values mapped onto the gray scale, thereby controlling contrast. A
wide WW displays a broader range of CT numbers, improving contrast between
different tissue types. Conversely, a narrow WW enhances the visibility of
subtle density differences within soft tissues but reduces overall
contrast.
Adjusting WL and WW helps optimize CT interpretation for various
anatomical targets such as bone, soft tissue, or air-filled cavities.
Discussion: Cerebral Palsy in Children
Cerebral Palsy (CP) is a movement and
posture disorder resulting from non-progressive brain damage or abnormal brain
development that occurs before birth, during birth, or in early infancy.
CP affects muscle control, coordination, balance, and overall motor skills.
Causes of CP:
- Prenatal or
Perinatal Brain Injury: Brain
damage during fetal development or delivery may result from trauma, oxygen
deprivation, or other stressors.
- Postnatal
Brain Injury: Injury due
to accidents, infections, or other causes during infancy can affect brain
development and increase the risk of CP.
CP manifests with varying severity and types, depending on the extent and
location of brain injury. Some individuals may have mild symptoms, while others
experience severe movement impairments.
Common Motor Symptoms of CP:
- Spasticity (muscle stiffness)
- Muscle
weakness
- Postural
instability
- Uncoordinated
or jerky movements
- Gait
abnormalities
- Fine motor
skill difficulties
Motor impairments can significantly affect activities of daily living.
However, comprehensive rehabilitation programs—including physical
therapy, occupational therapy, speech therapy, and assistive devices—can
help improve functional independence and quality of life. Treatment plans must
be individualized based on each patient's specific needs and clinical
presentation.




Comments
Post a Comment